|
Abstract:
Study Design
Clinical case series, a prospective study
Objective
The aim of this study is to demonstrate that Anterior Lumbar Interbody fusion is effective in treating L5 radiculopathy due to foraminal stenosis.
Summary of background data
Radiculopathy due to foraminal stenosis as a result of loss of disc height may not respond to traditional foraminotomy/neurolysis due to inability to improve cranio-caudal stenosis. Interbody techniques have been advocated to increase disc space height and hence relieve root compression.
Methods
Prospectively collected outcomes data for 27 consecutive patients undergoing single or double ALIF to treat L5 radiculopathy due to foraminal stensosis was reviewed. VAS, Oswestry and Roland Morris scores pre-operatively, at 3 and 6 months were complete for 24 of 27 patients (17 degenerative disc disease, 7 spondylolisthesis). A statistical package ( STATA) was used to calculate descriptive data and The Wilcoxin Signed Rank Test used to determine statistical significance.
Results
There was significant improvement noted in all the measured parameters including VAS which improved from a mean pre-op of 6.5 ( 95 % CI 5.9 - 7.1) to 1.3 ( 95% CI 0.8 - 1.8) at 3 months and 0.9 ( 95%CI 0.5 - 1.3) at six months ( p< 0.0000)
Conclusion
In conclusion our study has shown that ALIF is an excellent option for the treatment of L5 radiculopathy due to foraminal stenosis as results are consistent with a significant improvement in disability and pain.
J.Orthopaedics 2012;9(2)e3
Keywords:
Anterior lumbar interbody fusion; Foraminal stenosis; Degenerative disc; Spondylolisthesis Whilst most spinal surgeons are happy to perform anterior cervical discectomy and
fusion for upper limb radiculopathy due to foraminal discompromise, traditionally
most have viewed ALIF as a procedure for treatment of back pain. We present a small
case series of Anterior Lumbar Interbody Fusion using an implant packed with
autogenous bone graft for the treatment of L5 radiculopathy caused by foraminal
stenosis. We believe this is an excellent option to treat leg pain as a result of
foraminal stenosis caused by disc degeneration and spondylolisthesis.
Pathoanatomy
:
The anatomy of the lateral lumbar spinal canal and nerve roots has been described in
several studies (5,6,7) The normal and pathological anatomy as described by Crock
(5), the lumbar nerves emerge at their respective intervertebral foramina lying inferior
to the lumbar pedicle. The intervertebral foramen is bounded above and below by the
vertebral pedicles. Its floor from above downwards is formed by the postero-inferior
margin of the superior vertebral body, the intervertebral disc and the posterosuperior
margin of the inferior vertebral body. The roof is formed by the ligamentum flavum,
terminating at its outer free edge, and posteriorly lies the pars interarticularis and the
apophysial joint, formed between the adjacent inferior and superior vertebral facets.
The vertical height of the foramen is determined by the vertical height of the
corresponding intervertebral disc space. The development of foraminal stenosis is
related to the process of lumbar spondylosis. The loss of intervertebral disc height
secondary to desiccation and degeneration allows the superior articular process of the
inferior vertebra to subluxate anteriorly and superiorly, diminishing the area of the
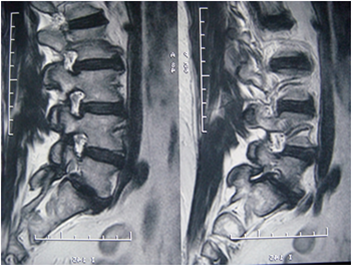
foramen (Fig.1).
An additional etiology of foraminal stenosis is craniocaudal
compression (“vertical stenosis”). Posterolateral osteophytes from the vertebral
endplates protrude into the foramen along with a laterally bulging annulus fibrosis or
herniated disc, compressing the nerve root against the superior pedicle (8)
Methods:
Prospectively collected outcomes data for 27 consecutive patients undergoing single
or double ALIF to treat L5 radiculopathy due to foraminal stensosis was reviewed. All
cases were selected and operated on by one surgeon.
VAS for pain assessment is a simple assessment tool consisting of a 10 cm line with 0
on one end, representing no pain, and 10 on the other, representing the worst pain
experienced, which a patient marks to indicate the severity of his or her pain (9)
The Oswestry Disability Index and Roland-Morris Questionnaire (RMQ) were used
to assess functional disability.
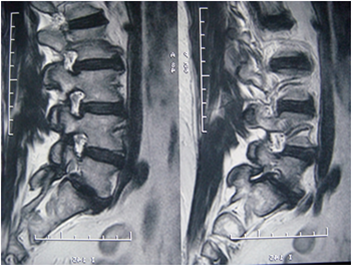
Radiological assessment was performed using erect plain x-ray and MRI scan
preoperatively.
Demographics
The number of patients in the study was 27, with 17 men and 14 women.
Unfortunately 3 patients were lost to follow up. The average age was 54.4 years and
the age ranged from 30 years to 76 years. Average follow-up period was 6 months.
Out of 24 patients available for a follow up 20 patients underwent single level ALIF
and 4 patients underwent two level ALIF
Types Of cases
Types
|
Sample size |
Degenerative Disc |
17 |
Spondylolisthesis |
7 |
Single Level |
20 |
Double level |
4 |
Operating time for single level
was from 100 – 195 minutes, the average time was 138.16 minutes. Length of stay in
hospital for a single level ALIF varied from 2 to 6 days, with an average of 3.3 days.
For a two level ALIF hospital stay varied from 4 to 5 days, with an average of 4.3
days.
Surgical Technique
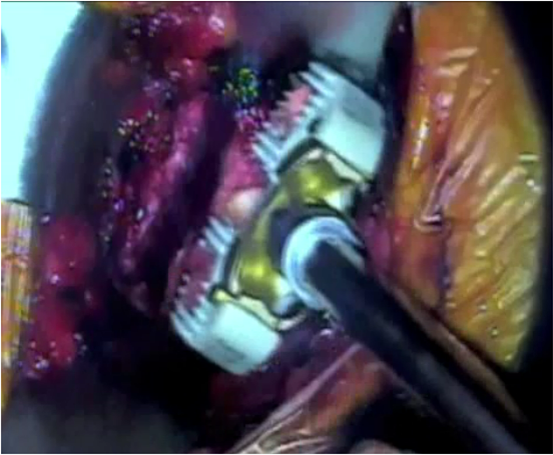
In all the cases a retroperitoneal approach to the anterior lumbar spine was performed
after harvesting autogenous graft from the right iliac crest. Following clearance of the
disc space a laminar spreader was introduced and a ronguer was used to clear the disc
annulus and osteophytes from the foramen. If the posterior annulus was solidly
calcified, a burr was used to achieve foraminal decompression. An interbody device
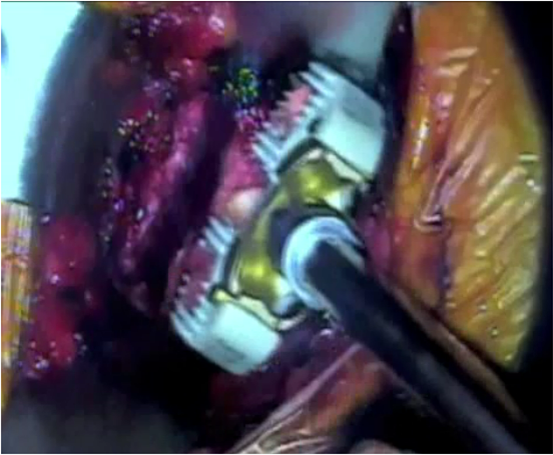
packed with the harvested graft was then secured by four screws in the
intervertebral space to restore disc height

Early in the series the operating
surgeon was concerned about the presence of the significant L4 disc degeneration and
undertook 2 level surgery in such cases. With subsequent procedures, the operating
surgeon became less concerned about adjacent level degenerative disc and was happy
to perform single level procedure.
Results
Complete data was available for 24 out of the 27 patients. Of the 3 lost to follow up
one had a bad outcome despite undergoing a technically successful procedure. He
withdrew from the study. A 2nd patient had an excellent clinical result from the
surgery based on post procedure follow-up. However, due to inadequate pre
procedure data the patient was excluded. The 3rd patient has been lost to follow up
and did not attend post procedure follow-up.
A statistical package (STATA) and the Wilcoxin Signed Rank Test were applied to
interpret the data. Of the 24 patients with complete data there was clinically and
statistically significant improvements in all measured parameters at 3 and 6 months
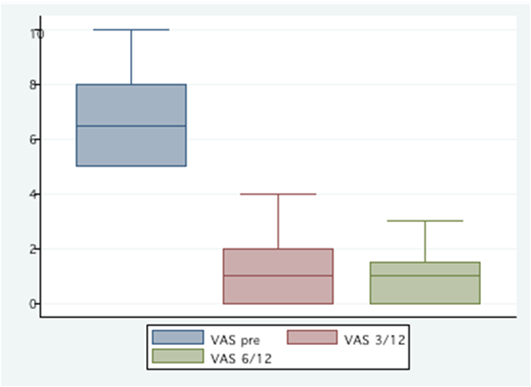
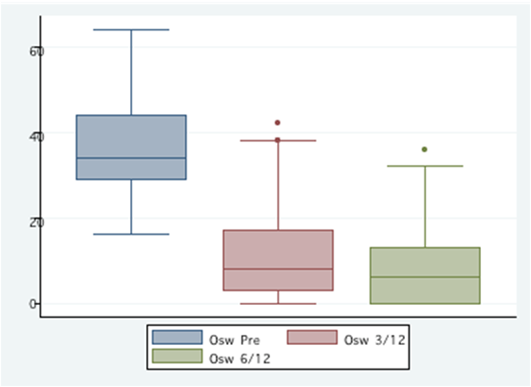
for both degenerative disc and spondylolisthesis cases (Table 2, 3&4). The VAS
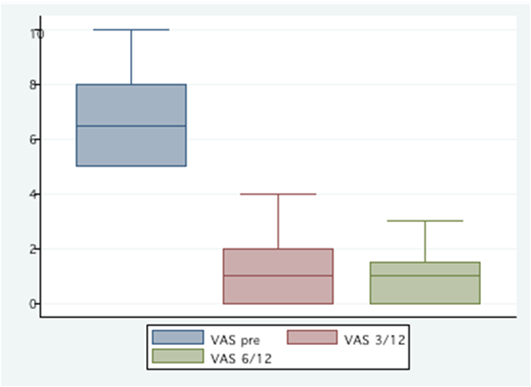
(Graph 1)
improved from a mean pre-op of 6.5 ( 95 % CI 5.9 - 7.1) to 1.3 ( 95% CI
0.8 - 1.8) at 3 months and 0.9 ( 95%CI 0.5 - 1.3) at six months ( p< 0.0000). Oswestry
scores
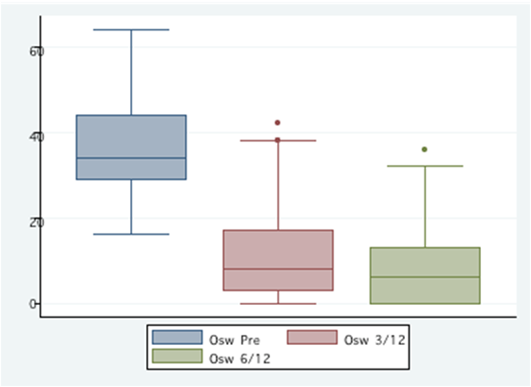
improved from a mean pre-op of 36.8 (95% CI 31.5 - 42.1) to 12.1
(95% CI 6.8 - 17.4) at 3 months and 8.8 ( 95%CI 4.4 - 13.2) at six months ( p<
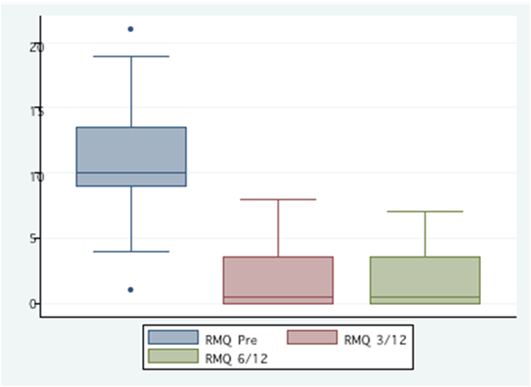
0.0000). Roland Morris scores
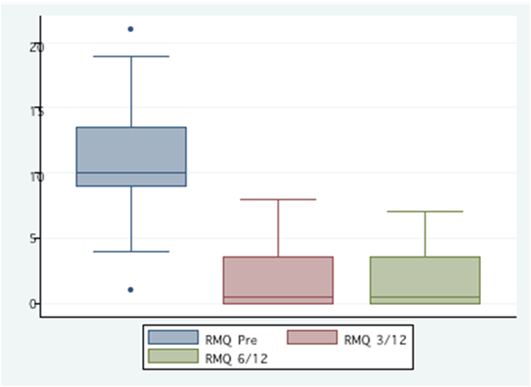
improved from a mean pre-op of 11.0 (95%
CI 9.1 - 12.9) to 1.9 (95% CI 0.8 - 3.0) at 3 months and 1.6 (95%CI 0.7 - 2.5) at six
months (p< 0.0000). Hospital stay, overall cost and complication rates are
favorable when compared to current available alternative surgical procedures.
Discussion
Loss of disc height results in the displacement of facets and an overall reduction in
size of intervertebral foramen (4) in a cadaveric study Hasegawa et al demonstrated
that a significant nerve root compression is associated with a foraminal height of less
than 15 mm and posterior disc height of 4 mm (14). A loss of disc height by 4 mm,
which is 35-50% of its normal height results in a reduction in the diameter of the
neuroforamen (15). Previous studies have shown a total increase in AP diameter after
anterior fusion appears to be directly related to the clinical outcome (16). A study by
Chan and Fay showed an increase in the volume of the neuroforamen by 22.9% for
L4-5 and 21.5% for L5-S1, the posterior disc height increased by 37.1 % at L4-5 and
45.1% at L5-S, following BAK instrumentation(4).
Anterior procedures that restore the height of the disc space can indirectly enlarge a
stenosed neuroforamen. Anterior interbody fusion also corrects mal-alignment of the
lumbar spine and reduces anterior slippage. The several advantages of anterior
interbody fusion(12) are direct observation of the anteriorly displaced vertebral body,
avoidance of damage to the posterior supporting ligaments, dura mater and nerve root;
reduced need for blood transfusion, early postoperative ambulation and a reduction
hospital stays, eradication of postoperative back pain and/or radiating pain; and a high
fusion rate (17,26)
Various previous studies have shown satisfactory clinical results for back pain with
anterior lumbar interbody fusion. (2,18,19,20,21,22)
Kim and Lee (18) reported no significant difference in clinical outcomes and fusion
rates between anterior interbody fusion and posterolateral fusion with transpedicular
fixation for isthmic spondylolisthesis in Adults.
Greenough et al (24) demonstrated
posterior instrumental fusion higher fusion rates (82%) compared (25) to anterior
fusion (76%) but with better clinical results in the latter procedure.
Pradhan’s (26) study showed the anterior approach to single-level lumbar fusion is
associated with less morbidity than the postero-lateral approach with no significant
difference in need for transitional facility care, complication rates, and given followup
period in radiographic fusion rate and clinical outcome.
Above mentioned studies have previously shown advantages of ALIF over other
procedures in terms of avoidance of damage to the posterior musculature, ligaments,
neural structures,
reduced need for blood transfusion, early postoperative ambulation
and reduced hospital stay.
In conclusion our study has shown that ALIF is an excellent option for the treatment
of L5 radiculopathy due to foraminal stenosis as results are consistent with a
significant improvement in disability, faster postoperative recovery, earlier return to
employment, reduced operating time and is more cost effective compared to other
available treatment options.
References:
Sidney Sacks, Anterior interbody fusion of the Lumbar spine: Vol. 47B JBJS 1965
A.Loguidice, R. Johnson, Anterior Lumbar Interbody Fusion: Spine Vol. 13 (3) 1988
Stephen D. Cook, PhD,* Laura P. Patron, Comparison of Methods for Determining the Presence and Extent of Anterior Lumbar Interbody Fusion: SPINE Volume 29, Number 10, pp 1118–1123
D. Chan, L. Fay, Increasing Neuroforaminal Volume by Anerior Interbody Distraction in Degenerative Lumbar Spine: Spine Vol.20(1) 1995
Crock H. Normal, pathologic anatomy of the lumbar spinal nerve root canals. J Bone Joint Surg [Br] 1981;63:487–90.
Hasegawa T, An H, Haughton V. Imaging anatomy of the lateral lumbar spinal canal. Semin Ultrasound CT MRI 1993;14:404–13
Bose K, Balasubramaniam P. Nerve root canals of the lumbar spine. Spine 1984;9:16–18.
Louis G. Jenis, Howard S. Spine Update Lumbar Foraminal Stenosis: SPINE Volume 25, Number 3, pp 389–394, 2000
Fairbank JC, Pynsent PB, "The Oswestry Disability Index." Spine 2000; 25(22):2940-2952
Fairbank JCT, Couper J, Davies JB. "The Oswestry low Back Pain Questionnaire." Physiotherapy 1980; 66: 271-273
Roland M, Morris R. A study of the natural history of low back pain. Part 1: Development of a reliable and sensitive measure of disability in low-back pain. Spine 1983;8:141–4.
Anterior Lumbar Interbody Fusion Indications for its Use and Notes on Surgical Technique H. V. CROCK, M.D., M.S., F.R.C.S., F.R.A.C.S. Clinical Orthopaedics Related Research,185 May. I982
Hasegawa T, An H, Haughton V, Nowicki B. Lumbar foraminal stenosis: Critical heights of the intervertebral discs and foramina. J Bone Joint Surg [Am] 1995;77:32–8.
Mayoux-Benhamou M, Revel M. A morhogenic study of the lumbar foramen – influence of flexion-extension movements and isolated disc collapse. Surg Radiology Anat 1989:11:97-102
Kim NH, Kim HK, Suh JS. A computed tomographic analysis of changes in the spinal canal after anterior lumbar fusion. Clin Orthop 1993;286:180–191.
*References (cited in order of appearance)
Harmon PH. Anterior excision and vertebral body fusion operation for intervertebral disk syndromes for the lower lumbar spine. Clin Orthop 1963;26:107–
Nam Hyun Kim, MD, and Jin Woo Lee, MD. Anterior Interbody Fusion Versus Posterolateral Fusion With Transpedicular Fixation for Isthmic Spondylolisthesis in Adults; SPINE Volume 24, Number 8, pp 812–817
Crock HV. Anterior lumbar interbody fusion: Indications for its use and notes on surgical technique. Clin Orthop 1982;165:157–63. 20)
Flynn JC, Hoque NA. Anterior fusion of the lumbar spine. J Bone Joint Surg [Am] 1979;61:111–43.
Inoue S, Watanabe T, Goto S, Tanahashi K, Takata K, Sho E. Degenerative spondylolisthesis: Pathophysiology and results of anterior interbody fusion. Clin Orthop 1988;227:90–8.
Sacks S. Anterior interbody fusion of the lumbar spine. Indication and results in 200 patients. Clin Orthop 1966;44:163–70
A Fujimaki, MD., H. V. Crock, M.D., M.S., F.R.C.S., F.R.A.C.S., SIRG Eorgem . Bedbrookm, M.S., F.R.C.S., F.R.A.C.S. The Results of 150 Anterior Lumbar Interbody Fusion Operations Performed by Two Surgeons in Australia Clinical Orthopaedii and Related Research : Number 165 May. 1982 (164-167)
Greenough, Charles G. MD; Peterson, Mark D. MD†; Hadlow, Simon FRACS; Fraser, Robert D. MD Instrumented Posterolateral Lumbar Fusion: Results and Comparison With Anterior Interbody Fusion Spine 1998 Feb 15;23(4):479-86 .
Greenough CG, Taylor LJ, Fraser RD. Anterior lumbar fusion: Results, assessment techniques and prognostic factors. Eur Spine J 1994;3:225-30 .
Pradhan, Ben B.; Nassar, John A.; Delamarter, Rick B.; Wang, Jeffrey C.Single- Level Lumbar Spine Fusion: A Comparison of Anterior and Posterior Approaches Journal of Spinal Disorders & Techniques: October 2002 - Volume 15 - Issue 5 - pp 355-361
|