|
Key words: Hip; Arthroplasty; Leg; Length; Discrepancy.
Competing interests: none declared, and no external funding received.
Sections:
- Abstract
- Main article
- Legends
- Bibliography
- Figures and tables
J.Orthopaedics 2011;8(1)e9
Abstract:
Introduction:
Limb length discrepancy (LLD) can lead to greater patients dissatisfaction and less favourable outcomes following hip replacement surgery. This study’s objective was to determine whether significant leg length inequality can be reduced using Charnley retractor pin and a reference point as a simple and cost effective intra-operative measurement technique. Methods: A retrospective analysis on a series of primary total hip arthroplasties (THA) was conducted. Patients with contralateral hip joint prosthesis were excluded. The nature and extent of pre and post-operative LLD was calculated from plain AP pelvis radiographs. We compared results in relation to the technique used for intra-operative measurement of leg length.
Results: 89 primary THA were analysed, mean patients age was 74 years (range 54 – 90 years). The mean postoperative LLD was 7.44 mm (range 0-29). 64% of patients resulted in long post-operative LLD, compared to 11% short LLD and 25% equal length. There was no statistically significant relationship between the extent of LLD pre-operatively and post-operatively (P=0.10). No difference was found between the type of prosthesis fixation (cemented, uncemented, hybrid) and the extent or nature of limb disparity. Pin measurement technique was used in 56 cases, compared to 33 cases where clinical assessment alone was performed. Statistical analyses were used to examine variation of LLD measurements. Despite the absence of significant differences in the extent or nature of LLD preoperatively across both groups, using the pin measurement was associated with lower LLD postoperatively with median LLD=4mm Inter Quartile Range (IQR 0-6), compared to clinical assessment alone with a median LLD=8mm (IQR 5-12) (P=0.001). Results revealed a greater proportion of limb equalisation when pin measurement was performed, 30% compared to 14%.
Conclusion: The measurement technique described is considered a useful adjunct in reducing leg-length discrepancy following primary total hip arthroplasty. It has the advantage of being simple, easily reproducible and at low cost.
Main article:
Introduction:
Leg length discrepancy (LLD) following total hip arthroplasty (THA) remains a controversial issue. Reports in the literature indicate greater patients dissatisfaction and less favourable functional outcomes following hip replacement surgery with limb length difference¹ ² ³. Nevertheless, the extent of limb disparity and how it is tolerated remains a highly subjective outcome. It has been previously noted that a third of patients report perceived LLD following primary THA4. Predominantly multifactorial, the effect of limb lengthening on surrounding structures is believed to be responsible. The literature does not report any exact lengthening as a reference measurement, however 9 mm or more of limb length discrepancy was perceived to be significant by patients and found to be associated with worse functional outcomes5. On the opposite, other authors have negated the association of leg length difference following primary total hip arthroplasty with poorer functional and patients satisfaction outcomes6. Nevertheless, it remains a major cause of litigation and patients show more dissatisfaction as a result of perceived leg length discrepancy7. This is especially true among female patients who tolerate less adaptive foot wear for LLD6. The principal goal of THA is to restore normal biomechanical parameters of the hip joint. Therefore, measurement of leg length remains an integral part in performing a successful THA. For the purpose of this study leg length discrepancy is defined as limb length disparity relative to the contralateral side. Several methods have been postulated with the aim of minimising LLD indirect methods such as preoperative templating and intraoperative radiographs, and direct methods of measuring limb length intraoperatively8 ?. The effectiveness of such techniques has been widely reported in the literature. Although radiographic measurement and templating is becoming more established, direct intraoperative measurement techniques are less familiar7. The perceived advantage in the use of direct intraoperative measurement is a stable reference point which remains constant throughout the crucial stages of the procedure. Hence it allows measurements to be taken and adjustment in limb length without the added costs. The principal objective of our study was to determine whether significant leg length inequality can be reduced with the utilisation of the technique proposed. We aim to introduce this technique as a safe and reliable adjunct to intraoperative measurement of limb length during primary total hip arthroplasty.
Methods:
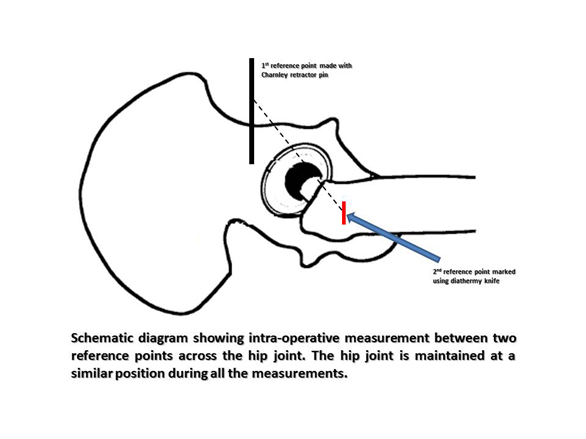
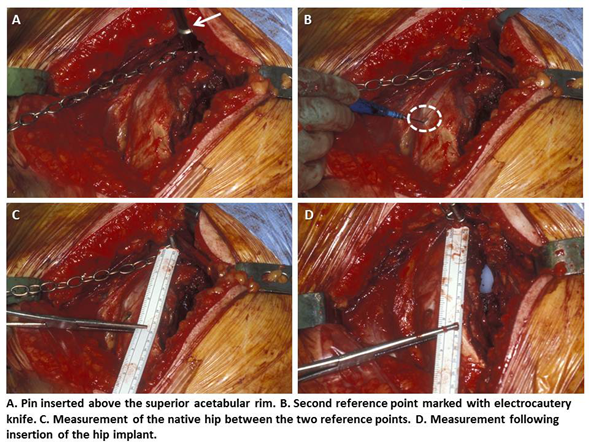
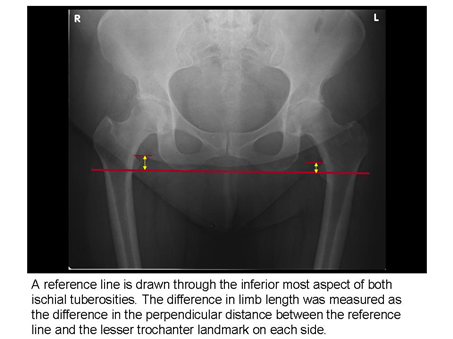
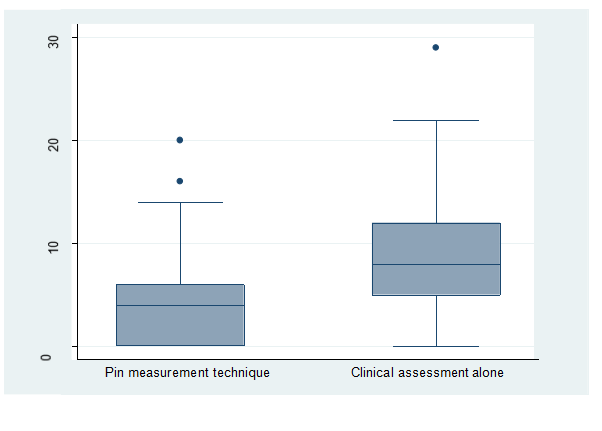
We conducted a retrospective analysis of 89 primary total hip arthroplasties and their associated pre and postoperative radiographs. The sample was divided into two groups depending on the methods used for equalisation of leg length, clinical assessment alone and clinical assessment combined with pin measurement technique described. For the purpose of this study we defined LLD as the radiographically calculated difference in length between the operated and the non-operated sides. Pre and Postoperative leg length discrepancy was calculated for both groups in order to establish whether significant disparity can be minimised using the intraoperative pin technique described. All procedures were performed by the same surgeon using his standard lateral (Hardinge) approach. We recorded demographic data, the type and extent of pre and post-operative LLD, and the type of hip prosthesis (Cemented: Exeter™ total hip system. Uncemented: Synergy™ femoral stem system Reflection™ cementless acetabular cup. Hybrid: Exeter™ femoral stem Reflection™ cementless acetabular cup). Patients were not assessed on their perception of LLD. We excluded patients who had contralateral hip joint prosthesis and patients with pre-existing hip joint anomalies which significantly affect LLD: developmental dysplasia, hip joint contractures, collapse of the femoral head, or acetabular erosion. Intraoperative measurement technique was carried out using a modified version of the reference pin method previously described by Mihalko et al?, McGee and Scott¹°, and Takigami et al¹¹. A non-threaded pin from Charnley Pin Retractor designed for intraoperative reflection of gluteal muscle was used. The pin was placed on the pelvis 2-3 cm proximal to the superior rim of acetabulum. The pin acts as a fixed point which remains constant throughout the procedure and is used as reference point for measuring distance. A second reference point, on the vastus tubercle on the lateral aspect of the greater trochanter was made using electrocautery knife (figure 1). Measurements were taken between the pin and the marked point prior to dislocation of the femoral head, during trialling of the implant and following the implant of the prosthesis (figure 2). The lower limb was placed in the same neutral hip joint position during each measurement. In addition, clinical assessment of leg length was made by comparing leg position and length relative to the contralateral side. Neck length was readjusted after insertion of the prosthesis so as to achieve intended leg length adjustment alongside adequate soft tissue tension. Measurements taken from the pre and post-operative radiographs were obtained using a validated technique5. We reviewed the anteroposterior (AP) radiographs of the pelvis. A reference line was drawn through the inferior margin of the two Ischial Tuberosities. On each side the perpendicular distance between the lesser trochanter landmark and the reference line was measured. Radiographic magnification was maintained at 1 to 1 using an electronic web based image archiving programme ‘Magic Web Siemens®’. All AP radiographs were taken with patient supine and in neutral position. In order to ensure appropriate rotation of the hips on the radiographs studied we assessed the alignment of the greater trochanters on both sides, the two lengths were compared and the difference recorded (figure 3). The calculated limb length difference was compared between the pre and post-operative radiographic measurements and the two groups of patients. The same observer carried out all measurements. In addition, re-measurements on the entire sample were taken by a second observer with blinding to the first set of results. The final results were recorded to the nearest millimetre if there were any differences between the two observers. The aim of all analyses was to examine how LLD measurements varied pre and post-operatively and to examine associations with other variables. In the analyses, the LLD values were treated in two different ways, as a continuous scale with the original values in mm, and categorical into three groups, nil, short and long. Spearman's rank correlation was used to examine the association between these measurements. The association between LLD measurements on a categorical scale was assessed using Fisher’s exact test. Due to the distribution of LLD values, non-parametric methods were used for the next set of analyses. The association between LLD measurements and leg length assessment technique was performed using the Mann-Whitney test. The association between LLD measurements and Hip prosthesis fixation method was performed using the Kruskal-Wallis test. Finally, Fisher's exact test was used to examine the association between the two categorical variables (length assessment technique and prosthesis), and LLD categories (nil, short and long).
Results:
There was a total of 89 primary total hip arthroplasties included in this study. All operations were performed by the same surgeon, the senior author of this article. Gender distribution was 32 male patients and 57 female patients, and the age range was between 54 and 90 years at the time of surgery, and with a mean age of 72 years (male=74, female=70). The types of total hip arthroplasties were as follows: 28% (n=25) uncemented, 20% (n=18) cemented and 52% (n=46) hybrid prostheses. Radiographic measurement of leg length discrepancy (LLD) on pre-operative plain film radiographs showed the following results for the affected side: Short leg 67% (n=60), long leg 16% (n=14), no LLD 17% (n=15). The mean pre-operative LLD was 7.62 mm with range of 0-35 mm. Radiographic measurement of leg length discrepancy (LLD) on post-operative plain film radiographs showed the following results for the operated side: Short leg 11% (n=10), long leg 64% (n=57), no LLD 25% (n=22). The mean post-operative LLD was 7.44 mm with range of 0-29 mm. The results did not demonstrate an association between leg length discrepancy and age or gender of the patients.
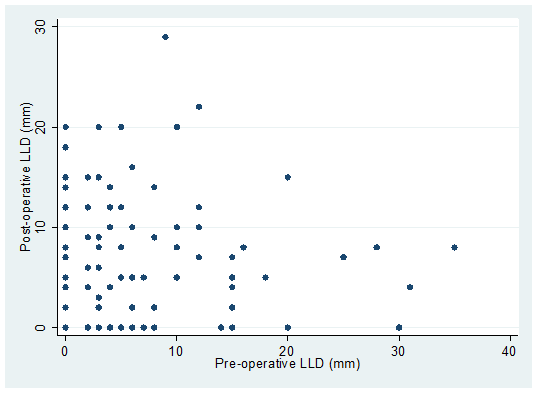
Analysis of the correlation between the pre-operative and post-operative radiographic measurements of LLD on a continuous scale demonstrated a skewed distribution but there was no association between pre and post-operative LLD (P=0.10). This distribution is outlined in the scatter plot graph (figure 4). Nevertheless, on a categorical scale more patients resulted in a long LLD relative to the contralateral side on post-operative radiographic measurement. These results were statistically significant (P <0.03). 93% of patients with a long LLD on pre-operative measurement resulted in a long LLD on post-operative measurement. This was closely followed by 86% patients who had no LLD on pre-operative measurement and resulted in a long LLD on post-operative measurement. These results are summarised in Table 1. The results also indicated that there was no statistically significant difference between type of arthroplasty prosthesis (uncemented, cemented or hybrid) and post-operative LLD measured radiographically. Table 2 summarises the results of post-operative LLD measurement in each prosthesis group. Table 3 shows the median and inter-quartile range (the interval containing the middle half of the data) for each of these groups.
In this study patients were divided into two groups according to the method utilised for assessing intra-operative leg length. There were 56 (63%) patients on whom intra-operative pin measurement technique and clinical assessment was used as described above, and 33 (37%) patients on whom clinical assessment alone was done by the surgeon by observation of leg length and position of both knees during the operation. The results showed no significant difference in the pre-operative radiographic measurement or nature of leg length discrepancy in the two groups, with an LLD median value of 5 mm in both groups. The methods utilised for assessing intra-operative leg length was associated with a significant difference in post-operative LLD measurements. In the group where the pin measurement technique was used we found a lower leg length discrepancy on post-operative measurement compared to the second group. The pin measurement technique resulted in a post-operative LLD median of 4 mm and Inter Quartile Range (IQR) of 0-6 mm. Compared to clinical assessment by the surgeon alone which resulted in post-operative LLD median of 8 mm and IQR of 5-12 mm (P=0.001). This is a statistically significant overall minimising of measured post-operative LLD with in the pin measurement technique group. These results are summarised in table 4 and graphically illustrated in the box plot (figure 5). The results showed no significant differences in the nature of leg length discrepancy between the two groups. Nevertheless, the group where pin measurement technique was used had a greater proportion of leg length equalisation compared to the second group, 30% (n=17) and 14 % (n=5) respectively. The proportion of short LLD on post-operative measurement was higher in the clinical assessment group compared to the pin measurement technique group, 17% (n=5) and 9% (n=5) respectively. Pre-operative equal leg lengths were 18% (n=10) in the pin measurement group and 15% (n=5) in the clinical assessment group, results are summarised in table 5.
Discussion:
Primary total hip arthroplasty remains an exceptionally cost effective and successful operation. Limb length inequality is among the most common complications with an impact on functional outcomes and long term success¹ ³. It is widely reported that about a third of patients perceive leg length discrepancy following primary THA¹ ³ ¹². The extent of LLD and whether this requires further intervention remains a controversial issue. The aim of THA however is to restore normal hip joint geometry, and surgeons most often attempt to achieve a stable hip joint at the cost of increasing limb length. Although an absolute limb equalisation is idealistic, an optimal situation would consist of the least significant post-operative LLD achievable.
This study did not aim to establish correlation between extent of limb length disparity and patients’ outcomes. Measurements were taken in order to analyse the effectiveness of intra-operative measurement techniques in reducing post-operative LLD. In this series a significant proportion of patients had a short LLD (67%) on pre-operative measurements relative to the contralateral side. This is believed to be consistent with the anatomical changes observed with osteoarthritis of the hip joint. An important proportion of patient (64%) resulted in a long LLD on post-operative measurements. This is believed to be consistent with the lengthening and soft tissue tension required in order to achieve stability of the prosthetic joint. In the extent of limb length changes, the mean post-operative LLD on radiographic measurements was 7.44 mm. These results correlate to the range of post-operative LLD reported in previous large scale studies, which varies from 1 mm to 16 mm7 ¹¹. In the group where intra-operative pin measurement technique had been used the majority of cases were not lengthened or shortened by more than 6 mm with a resultant mean post-operative LLD of 5 mm. This is important to highlight, since previous reports have indicated that length disparity was perceived by patients post-operatively once it exceeded 6 mm7 ¹³. Although the change from pre to post-operative LLD demonstrated was not significant, an overall reduction of post-operative LLD with the use of pin measurement technique was notable. In this series there was no correlation between the pre and post-operative LLD and no association between the extent of LLD, age, gender or type of prosthesis (cemented, uncemented, hybrid). The results did not show a significant difference in these parameters between the two groups of intra-operative length assessment methods.
The use of clinical assessment of length alone is a subjective estimation dependent on the surgeon’s observation and affected by the position of the patient and position of the limb. Relying on clinical assessment alone leads the surgeon to reside on the side of caution and attempt to produce more soft tissue tension by over lengthening the limb. Adding an objective measurement method as described in this study helps achieve the balance between sufficient prosthetic joint stability and excessive lengthening. Intra-operative clinical assessment alone resulted in length discrepancy in 86% of patients, compared to 70% of patients when the pin measurement technique was also utilised. The use of metric measurement systems in the intra-operative assessment of leg length during primary THA is relatively well described in the literature and various techniques have been put forward¹° ¹4. These techniques appear to be more elaborate and more invasive, requiring a separate skin incision and different entry point. The use of larger constructs can be more difficult to assess and requires observation from a distance. In addition, accurate position of the pins used in the length assessment is crucial in the success of those techniques previously described. The use of Steinmann pins has also been shown to be associated with loosening during the procedure¹5. These techniques are therefore believed to add time and cost to the operation. In contrast, the technique described in this study is simpler to use and more easily reproducible. The Charnley retractor pin inserted proximally has a low profile and does not interfere with the surgical technique. It does not require extended or separate skin incision. The pin remains stable throughout the operation and does not require accurate position since it is simply used as reference point. No distal pin is used which can potentially interfere with the surgical technique. In this series no intra-operative complications resulted from the use of the pin measurement technique.
In conclusion, the use of intra-operative pin measurement technique helped reduce the extent of post-operative leg length discrepancy measured on plain film radiographs. The technique as used by the authors was associated with a reduced LLD and a greater proportion of limb length equalisation following primary THA. Several methods are described and available to the surgeon to help restore limb equalisation during this procedure, choice of method is often influenced by accuracy, ease of use, potential added risks and costs. We believe that our method fulfils these important factors. It is crucial to highlight that impeccable surgical technique and correct positioning of the implant components remain the first priority. In order to achieve optimal minimising of LLD following primary THA, a combination of our technique with careful pre-operative planning and thorough clinical assessment is recommended. Further studies are required in order to determine the impact of this technique on functional outcomes and patients perception of leg length discrepancy complications.
Legends:
Figure 1: Intraoperative measurement schematic diagram using the pin retractor method as a stable reference point.
Figure 2: Intraoperative pictures of the measurement technique using the pin retractor method as a stable reference point.
Figure 3: Plain film radiographic measurement of limb length discrepancy.
Figure 4: Scatter plot showing distribution of pre and post-operative LLD measurements in mm.
Figure 5: Box plot showing post-operative LLD measurement (mm) in the two groups of operative leg length assessment.
Table 1: The association between pre and post-operative LLD.
Table 2: Post-operative LLD measurement in each prosthesis group.
Table 3: Post-operative LLD measurement in each prosthesis group, median & inter-quartile range (IQR).
Table 4: Post-operative LLD measurement in the two groups of operative leg length assessment technique.
Table 5: Post-operative LLD measurement in each operative leg length assessment technique.
Reference:
Williamson JA, Reckling FW. Limb length discrepancy and related problems following total hip replacement. Clin Orthop 1978;134:135-8.
Jasty M, Webster W, Harris W. Management of limb length inequality during total hip replacement. Clin Orthop 1996;333:165-71.
Edeen J, Sharkey PF, Alexander AH. Clinical significance of leg-length inequality after total hip arthroplasty. Am J Orthop 1995;24:347-51.
Woolson ST, Hartford JM, Sawyer A. results of a method leg length equalisation for patients undergoing primary hip replacement. J Arthroplasty 1999;14:159-64.
Hofmann AA, Bolognesi M, Lahav A, Kurtin S. Minimizing leg-length inequality in total hip arthroplasty: use of preoperative templating and intraoperative xray. Am J Orthop 2008;37:18-23.
White TO, Dougall TW. Arthroplasty of the hip: leg length is not important. J Bone Joint Surg [Br] 2002;84:335-8.
Konyves A, Bannister GC. The importance of leg length discrepancy after total hip arthroplasty. J Bone Joint Surg [Br] 2005;87:155-7.
Clark CR, Huddleston HD, Schoch EP, Thomas BJ. Leg length Discrepancy after total hip arthroplasty. J Am Acad Orthop Surg 2006;14:38-45.
Milhalko WM, Phillips MJ, Krackow KA. Acute sciatic and femoral neuritis following total hip arthroplasty: a case report. J Bone Joint Surg [Am] 2001;83:589-92.
McGee HMJ, Scott JHS. A simple method of obtaining equal leg length in total hip arthroplasty. Clin Orthop 1985;194:269-70.
Takigami I, Itakazu M, Itoh Y, Matsumoto K, Yamamoto T, Shimizu K. Limb length measurement in total hip arthroplasty using a callipers dual pin retractor. Bull NYU Hosp Joint Dis 2008;66(2):107-110.
Wylde V, Whitehouse SL, Taylor AH, Pattison GT, Bannister GC, Blom AW. Prevalence and functional impact of patient-perceived leg length discrepancy after hip replacement. Int Orthop 2009;33:905-9.
Sarrongi PP, Bannister GC. Leg length discrepancy after total hip replacement. Hip 1997;7:121-4.
Woolson ST, et al. Leg length equalisation during total hip replacements. Orthopedics 1990;13(1):17-21.
Shiramizu K, et al. L-shaped calipers for limb length measurement during total hip arthroplasty. J Bone Joint Surg [Br] 2004;86:966-9.
Figures and Tables:
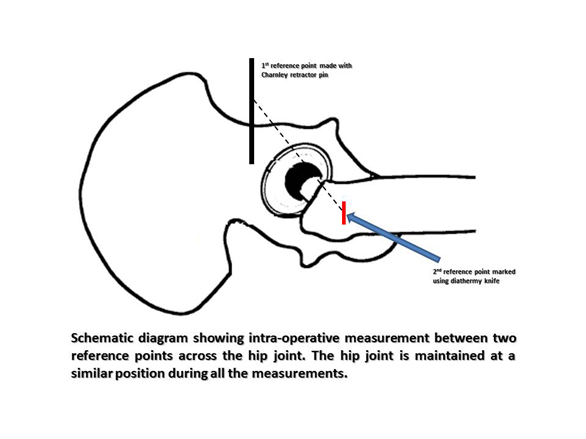
Figure 1: Intraoperative measurement schematic diagram using the pin retractor method as a stable reference point.
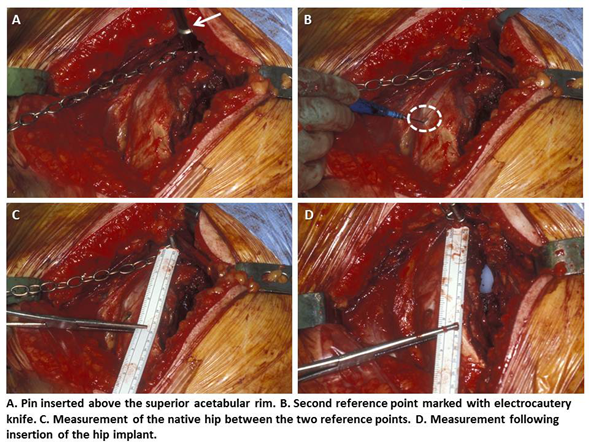
Figure 2: Intraoperative pictures of the measurement technique using the pin retractor method as a stable reference point.
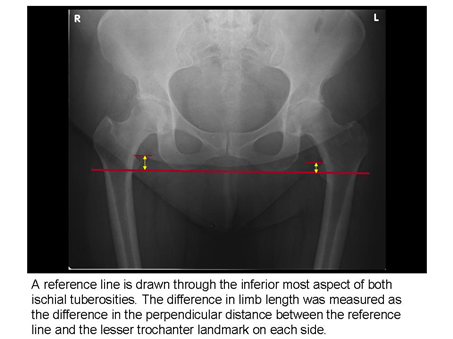
Figure 3: Plain film radiographic measurement of limb length discrepancy.
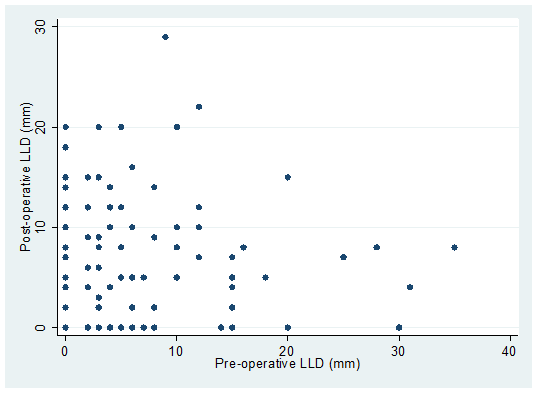
Figure 4: Scatter plot showing distribution of pre and post-operative LLD measurements in mm.
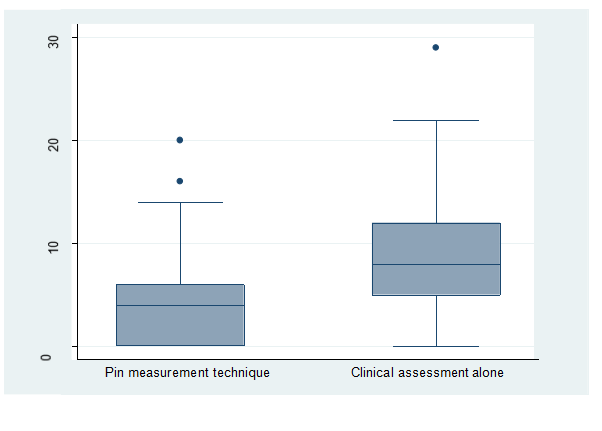
Figure 5: Box plot showing post-operative LLD measurement (mm) in the two groups of operative leg length assessment.
|
Post-operative LLD |
P-value |
Pre-operative LLD |
Nil
N (%) |
Short
N (%) |
Long
N (%) |
|
Nil |
1 (7%) |
1 (7%) |
13 (86%) |
<0.03 |
Short |
20(33%) |
9 (15%) |
31 (52%) |
Long |
1 (7%) |
0 (0%) |
13 (93%) |
Table 1: The association between pre and post-operative LLD.
Variable |
Category |
Nil
N (%) |
Short
N (%) |
Long
N (%) |
P-value |
Prosthesis |
Cemented |
5 (28%) |
1 (5%) |
12 (67%) |
0.80 |
Uncemented |
7 (28%) |
3 (12%) |
15 (60%) |
Hybrid |
10 (22%) |
6 (13%) |
30 (65%) |
Table 2: Post-operative LLD measurement in each prosthesis group.
Variable |
Category |
LLD
Median (IQR) |
P-value |
Prosthesis |
Cemented |
5 (2, 8) |
0.42 |
Uncemented |
5 (0, 12) |
Hybrid |
7.5 (4, 12) |
Table 3: Post-operative LLD measurement in each prosthesis group, median & inter-quartile range (IQR).
LLD measurement |
Variable |
Category |
LLD
Median (IQR) |
P-value |
Pre-operative LLD |
Technique |
Pin technique |
5 (2, 12) |
0.35 |
Clinical assessment only |
5 (3, 6) |
Post-operative LLD |
Technique |
Pin technique |
4 (0, 6) |
0.001 |
Clinical assessment only |
8 (5, 12) |
Change from
Pre to Post- operative |
Technique |
Pin technique |
0 (-5, 4) |
0.34 |
Clinical assessment only |
0.5 (-5, 10) |
Table 4: Post-operative LLD measurement in the two groups of operative leg length assessment technique.
Variable |
Category |
Nil
N (%) |
Short
N (%) |
Long
N (%) |
P-value |
Pre-operative LLD |
Pin technique |
10 (18%) |
37 (66%) |
9 (16%) |
0.95 |
Clinical assessment |
5 (15%) |
23 (70%) |
5 (15%) |
Post-operative LLD |
Pin technique |
17 (30%) |
5 (9%) |
34 (61%) |
0.18 |
Clinical assessment |
5 (14%) |
5 (17%) |
23 (69%) |
Table 5: Post-operative LLD measurement in each operative leg length assessment technique.
|