Address for Correspondence
Lorraine H. Hutzler, BA (First Author, Corresponding Author)
301 East 17th Street, Suite 1402
New York, NY 10003
(212) 598-6048
(212) 598-3883 (Fax)
lorraine.Hutzler@nyumc.org
Abstract
Hospitals are increasingly incorporating nasal screening and decolonization programs into their routine pre-surgical testing protocol for patients at high risk of developing surgical site infections (SSI’s). Mupirocin ointment or povidone-iodine applied to the nares prior to surgery may be equally effective in short term Staphylococcus aureus decolonization. Evidence shows that nasal colonization is a risk factor for SSI’s and there is mounting evidence that decolonization is a potential strategy for decreasing infection rates in the orthopaedic population. Screening and decolonization of S. aureus infections may reduce the need for revision surgeries, additional hospitalizations, use of intravenous antibiotics and decrease the incidence of recurrent infections. Studies have demonstrated high potential cost savings associated with screening and decolonizing patients prior to high risk orthopaedic procedures (1, 2). However, due to the large number of patients needed to achieve statistical significance, further studies are necessary to determine the precise role and optimal protocol for screening and decolonization of S. aureus prior to high-risk orthopaedic procedures.
J.Orthopaedics 2011;8(3)e8
Keywords:
Surgical Site Infection; Nasal Screening; Decolonization; Cost Savings
Introduction:
Overview of Adapting Nasal Decolonization Programs
Many hospitals are making nasal screening and decolonization programs part of their routine pre-surgical testing protocol. The proportion of revisions due to infection is projected to rise for the next 25 years, and the economic burden of infections is expected to exceed 50% of the inpatient resources available for revision arthroplasties in 2016 and 2030 for total hips and knees, respectively. In addition to the direct costs of infection, states are now requiring health care facilities to publicly report certain health-care associated infections. Screening and decolonization of S. aureus infections may reduce the need for revision surgeries, additional hospitalizations, use of intravenous antibiotics and the incidence of recurrent infections. The high cost of treating an orthopaedic implant infection makes any intervention, such as decolonization, that potentially reduces the risk very likely to be cost saving. Furthermore, SSI rates are increasingly being used as hospital quality metrics and patients preparing to undergo elective surgery are now able to evaluate their providers based upon outcomes and infection data. Insurance companies are likely to select participating hospitals or provide higher reimbursement to institutions which consistently show best practices and outcomes. Consequently, prevention of infection is paramount for an institution’s reputation and financial health (1). In this review, we evaluate the literature evidence and our institution’s experience for the effectiveness of nasal screening and decolonization a part of the effort for the prevention of surgical site infections in the high risk orthopaedic population.
Epidemiology
The nares are commonly colonized by S. aureus. Approximately 20% of individuals are chronically colonized with a single strain of S. aureus, and are called persistent carriers. A large proportion of the population (60%) harbors S. aureus intermittently, and the strains change with varying frequency. Such people are called intermittent carriers. Finally, a minority of patients (20%) almost never carries S. aureus and are called noncarriers. Persistent carriage is more common in children than adults, and many people change their pattern of carriage between the age of 10 and 20 years. The reasons for these patterns are unknown. Persistent carriage seems to have a protective effect on the acquisition of other strains during hospitalization (3). However, carriers are 2 to 9 times more likely to acquire S. aureus SSI’s than noncarriers. In fact, nasal carriage is the only independent risk factor for S. aureus SSI in patients undergoing orthopaedic implant surgery (4, 5). Although the prevalence of nasal carriage may vary depending on the population, many studies show an increase in colonization by methicillin-resistant S. aureus (MRSA) over the past decade.
Evidence of Effectiveness of Decolonization Regimens
Although staphylococci are common inhabitants of the skin and mucus membranes, the anterior nares provide the principal reservoir for these organisms (6). There is a strong epidemiologic association between nasal carriage of S. aureus and development of S. aureus SSI’s. Carriage of MRSA constitutes a special problem with regard to prevention and treatment of infection. Elimination of nasal carriage would theoretically reduce the infection rates in populations in which it has been identified as a risk factor (3). When the nares are treated topically to eliminate nasal carriage, in most cases the organism also disappears from other areas of the body. In a study performed by Ammerlann et al. (7) short-term nasal application of mupirocin was the most effective treatment for eradicating methicillin-resistant S. aureus carriage, with an estimated success rate of 90% 1 week after treatment and approximately 60% after a longer follow-up period.
Colonization of Providers
Physicians have a higher prevalence of MSSA colonization compared to the general population but an equivalent prevalence of MRSA. Studies have shown that 10-15% of healthy adults carry S. aureus in their nares; this figure rises to 20-35% in hospital personnel (6, 8). This puts hospital personnel at risk for developing SSI’s during their own elective surgery and raises concerns about spread to patients under their care.
A study by Vonberg et al (9) showed 3% of MRSA outbreaks were caused by asymptomatic colonized healthcare workers and demonstrated that healthcare workers are capable of transmitting MRSA to others making colonization a potential concern. Other studies have shown that the incidence of nasal colonization with S. aureus among attending orthopaedic physicians is similar to the prevalence found in their high risk patient population. The prevalence of S. aureus in the residents was even greater than the attendings. This is postulated to the amount of time residents spend in the hospital on the floors caring for patients (10). It is known that different surgeons can have different infection rates, and it has been shown that infection surveillance of individual surgeons leads to lower infection rates (11). However there is no evidence to suggest that nasal decolonization of surgeons is effective in preventing SSI’s in patients.
Evidence that Decolonization Reduces SSI Rates
(See Table 1)
A randomized double-blinded, placebo-controlled multi-center trial by Bode et al. (12) demonstrated a decrease in the rate of deep SSI’s acquired in the hospital following rapid screening and decolonization on admission of nasal carriers of S. aureus. A total of 1,270 nasal swabs from 1,251 patients were positive for S. aureus, of these 917 were enrolled in the intention-to-treat analysis, with 808 (88.1%) undergoing a surgical procedure. The rate of S. aureus infection was 3.4% (17 of 504 patients) in the decolonized group, as compared with 7.7% (32 of 413 patients) in the placebo group that was not decolonized (P=0.005). The authors concluded that the number of surgical-site S. aureus infections acquired in the hospital can be reduced by rapid screening and decolonizing of nasal carriers of S. aureus on admission. Germatt et al. (13) studied the effect of prophylactic mupirocin treatment in the orthopedic population in an unblinded interventional trial. The wound infection rates were 14/1,044 in the intervention group treated with mupiricon, and 34/1,260 in the control group not treated with mupirocin (P = 0.02). A prospective observational study of decolonized patients performed by Rao et al. (14) found the overall infection rate, including nonstaphylococcal infections, decreased from 2.6% during the preintervention period to 1.5% during the intervention period (P=0.02) and concluded that preoperative nasal decolonization is a safe way to reduce S. aureus SSI's in patients undergoing TJA.
Two additional studies performed by Kluytmans et al. in non-orthopaedic populations also found nasal decolonization using mupirocin ointment to be effective in reducing S. aureus infections. The first study by Kluytmans et al. (15) consisted of a historical control group and an intervention group of cardiothoracic surgery patients. The historical control group consisted of 928 patients and the intervention group of 868, of whom 752 were treated with mupirocin. In the intention-to-treat analysis, a significant reduction in SSI rate was observed after the intervention (historical-control group 7.3% and intervention group 2.8%; (P < .0001). The SSI rate in the concurrent control group was also significantly higher than in the treated group (7.8% and 2.0%, respectively; P = .0023). They concluded that perioperative elimination of nasal carriage using mupirocin nasal ointment significantly reduces the SSI rate in cardiothoracic surgery. The second study was comprised of 226 hemodialysis patients, of whom 172 were evaluated to determine the efficacy of mupirocin on preventing bacteremia (16). Sixty-seven (39%) were identified as nasal carriers. Following the initial treatment, 66 nasal cultures (98.5%) became negative. After 3 months and 6 months, respectively, 63 (94%) and 61 (91%) of the treated carriers had negative cultures. The rate of bacteremia (defined as the number of episodes of S. aureus bacteremia per patient-year on hemodialysis) was significantly lower among the 226 patients in the study group (0.04 per patient-year) than among the 273 patients in the control group (0.25 per patient year, P < .001). They concluded mupirocin nasal ointment effectively eliminates nasal carriage of S. aureus in patients on hemodialysis and reduced the incidence of bacteremia in this population.
Financial Implications of Surgical Site Infectio
ns
Total joint and spine fusion patients are orthopaedic populations at high risk for infection. There were approximately 658,000 primary joint arthroplasties performed in the United States in 2005 and 79,000 revisions in the same year. This number is projected to rise to 4 million primary arthroplasties and 375,000 revisions by the year 2030. Infection rates after hip and knee arthroplasty were reported to be 1.7% and 2.1%, respectively, when post discharge surveillance was conducted, and the percentage of revisions that were the result of deep infections was estimated at 8.4% for hips and 16.8% of knees in 2005 (1). The proportion of revisions due to infection is projected to rise for the next 25 years, and the economic burden of infections is expected to exceed 50% of the inpatient resources available for revision arthroplasties in 2016 and 2030 for total hips and knees, respectively. Simultaneously, according to the Healthcare Cost and Utilization Project databases, the number of spinal fusion procedures had an exponential increase of 73%, from 202,100 procedures performed in 1997 to 349,400 procedures in 2005. The incidence of postoperative spine infections has been reported to be as high as 15%, with higher risks noted for revision spinal surgeries. The average cost of a septic joint revision is $70,000 and the average cost of treating a spine infection is $100,000 (see Figure 2). Therefore, successful efforts to reduce infections associated with these procedures are likely to have a significant impact. A decision analysis study demonstrated this potential cost savings with screening and decolonization of patients before elective arthroplasty and spine fusion procedures. Comparing the cost of screening to the cost of infection investigators found screening and decolonization became cost effective when the relative rate of SSI decreases by just 10% (1). This effect is due to the high cost of treating SSI’s after these high risk orthopaedic procedures in comparison to the low cost of a screening and decolonization program (1).
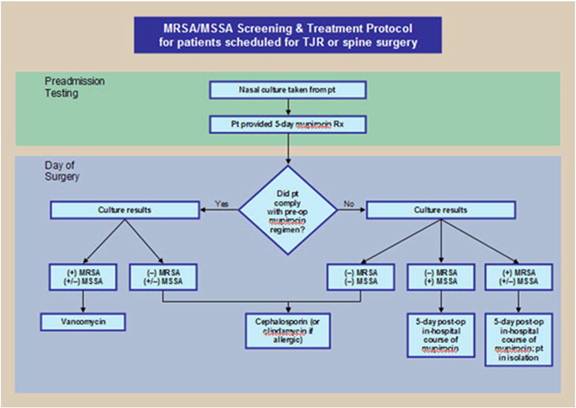
NYUHJD Algorithm for Decolonization
Our institution implemented a S. aureus screening and decolonization program for patients undergoing primary hip or knee arthroplasty and spine fusion (see Figure 1). All patients who went through the hospital’s pre-admission testing program participated in the study. Patients were given a prescription for mupirocin ointment and received a nasal culture preoperatively. If the patient complied with the mupirocin treatment and the nasal cultures were positive for MRSA, they received peri-operative antibiotic prophylaxis with vancomycin. In addition, they received in hospital decolonization with mupirocin and were treated with isolation precautions after surgery to protect against the spread of MRSA in the hospital. If they were noncompliant and had cultures positive for MSSA, they were treated peri-operatively with traditional prophylaxis with a cephalosporin and were decolonized peri-operatively with mupirocin. All patients with negative cultures for both MRSA and MSSA received traditional cephalosporin treatment perioperatively (1).
NYUHJD Results and Acceptance of Algorithm for Decolonization
As seen in the study by Kim et al. implementation of an institution wide prescreening program for the identification and eradication of MRSA carrier status of patients undergoing elective orthopaedic surgery is feasible and can lead to significant reductions in postoperative rates of surgical site infections (2). At our institution we investigated the effects of implementation of an institution wide screening, decolonization and prophylaxis protocol on the rates of SSI’s in patients undergoing primary knee and hip arthroplasties. 2,058 patients were enrolled in the study, 1,644 patients were in the treatment group and 414 were in the concurrent control group. The treatment group attended pre-operative admission testing (PAT) clinic where they were screened for MSSA and MRSA colonization. All patients were provided a 5-day course of nasal mupirocin for decolonization and a single pre-operative chlorhexidine shower. Additionally, patients colonized with MRSA received vancomycin peri-operative prophylaxis. The concurrent control group did not attend PAT or receive mupirocin treatment, they received either cefazolin or clindamycin for perioperative antibiotic prophylaxis, as their carrier status was unknown. All other peri-operative infection control measures were identical for the two groups. There were a total of 6 deep S. aureus infections in the control group (1.45%) and 21 in the treatment group (1.28%), this represented a decrease of 13% (P=0.809) in the treatment versus control group. This decrease represented an encouraging positive trend that supports the use of pre-operative colonization testing, but did not reach statistical significance due to control group sample size limitations. Therefore, further study will be needed to determine if our program demonstrates statistically significant results that are similar to those found by previous investigators. However, we did experience a significant reduction in hospital acquired MRSA infections after the decolonization program was initiated. The rate (per 1000 patient days) of hospital acquired MRSA infections was 0.05% before the decolonization program was initiated and fell to 0.029% after the initiation of our program (P= 0.007) (see Figure 3).
Patient Attitude and Compliance
We also assessed patient attitude and compliance with the decolonization program. Surgical patients at our hospital’s Pre-Admission Testing Clinic (PAT) received S. aureus reduction protocols instructing the preoperative use of chlorhexidine gluconate (CHG) soap and intranasal mupirocin ointment (MO). A survey was distributed to patients participating in the program. 81% of those who submitted survey responses indicated they had followed the MO protocol (MO users) while 89% indicated they followed the protocol for CHG (CHG users). However, 54% of MO users reported an out of pocket expense ranging from $2-$115 with a mean of $31, and 13% of MO users indicated the expense was a hard or very hard financial burden. 6% of MO users reported difficulty in locating the MO. In addition, 93% of CHG users reported CHG was very easy to use. Compliance despite potential barriers indicates a concern with infection and demonstrates a motivation for performing infection prevention measures. However, in this study, only 46% of respondents indicated a concern with SSI, suggesting further efforts at patient education are necessary. Improved compliance may be achieved if MO were provided to those patients with high out of pocket expenses or those who had difficulty purchasing or locating the product (17).
Future Directions
PCR or molecular testing may become more widely available for the screening of S. aureus colonization. Molecular testing allows rapid turnaround time and enables the physician to prescribe the decolonization regimen to only those patients who are S. aureus carriers. This may enable more discreet use of antibiotics, potentially decreasing the risk of antibiotic resistance. In addition, alternative decolonization protocols may become available due to the current expense associated with mupirocin. This substitution of povidone-iodine for mupirocin represents a significant potential cost savings as the average cost of a course of povidone-iodine is $5, while the average cost of a course of mupirocin ointment is $95, provided it can be established that it is as effective in decolonization and reducing the incidence of SSI rates with orthopaedic surgery.
Summary
Hospitals are increasingly implementing nasal screening and decolonization programs as part of their routine pre-surgical testing protocol due to mounting positive evidence that reductions in SSI rates can be achieved with this relatively low cost intervention. Screening for S. aureus infections potentially reduces the need for revision surgeries, additional hospitalizations, IV antibiotics and they may decrease the incidence of recurrent infection. However, due to the large number of patients needed to achieve statistical significance, further studies are necessary to determine the precise role and optimal protocol for screening and decolonization of S. aureus prior to high risk orthopaedic procedures.
Appendix
Table 1: Mupirocin Studies
Study |
# of Patients |
Type of Study |
Result |
Bode LG, et al.
N Engl J Med. 2010 Jan 7; 362(1):9-17. |
6,771 |
Randomized, double-blind, placebo-controlled clinical trial |
The rate of S. aureus infection was 3.4% (17 of 504 patients) in the mupirocin–chlorhexidine group, as compared with 7.7% (32 of 413 patients) in the placebo group. |
Germaat-van der Sluis AJ, et al.
Acta Orthop Scand. 1998; 69:412-4. |
2,304 |
Unblinded Intervention Trial |
The wound infection rates were 14/1,044 in the intervention group and 34/1,260 in the control group (p = 0.02). |
Rao N, et al.
Clin Orthop Relat Res. 2008; 466:1343-8. |
636 |
Prospective Observational Study |
The overall infection rate decreased from 2.6% during the preintervention period to 1.5% during the intervention period. |
Kluytmans JA, et al.
Infect Control Hosp Epidemiol. 1996; 17:780-5. |
1,796 |
Historical control group and intervention group |
In the intention-to-treat analysis, a significant reduction in SSI rate was observed after the intervention (historical-control group 7.3% and intervention group 2.8%; P < .0001). The SSI rate in the concurrent control group was significantly higher than in the treated group (7.8% and 2.0%, respectively; P = .0023). |
Kluytmans JA, et al.
Infect Control Hosp Epidemiol. 1996;17:793-7 |
226 |
Prospectively followed cohort |
The rate of was significantly lower in the study group (0.04 per patient-year) than among the 273 patients in the control group (0.25 per patient year, P < .001). |
Figure 1. Screening Algorithm
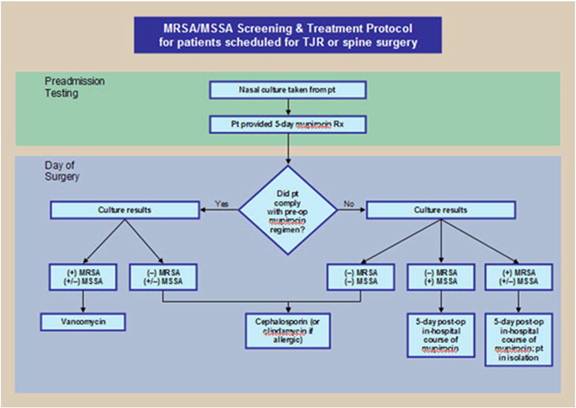
Figure 2. Cost Parameters
Parameter |
|
|
|
Mupirocin Treatment |
$90 |
Nasal Culture |
$20 |
Vancomycin Prophylaxis |
$4 |
Primary Total Joint |
$15,000 |
Revision of Infected Total Joint |
$70,000 |
Spine Surgery |
$50,000 |
Revision of Infected Spine Surgery |
$100,000 |
Figure 3. Comparison MRSA Rates/1000 Patients
(P=0.007)
Reference :
1 Slover J, Haas J, Quirno M, Phillips MS, Bosco J. Cost-Effectiveness of a Staphylococcus aureus Screening and Decolonization Program for High-Risk Orthopaedic Patients. The Journal of Arthroplasty. 2010 Mar. Level I.
2 Kim DH, Spencer M, Davidson SM, Ling Li, et al. Institutional Prescreening for Detection and Eradication of Methicillin-Resistant Staphylococcus aureus in Patients Undergoing Elective Orthopaedic Surgery. The Journal of Bone and Joint Surgery (American) 2010; 92:1820-6. Level I.
3 Kluytmans J, van Belkum A, Verbrugh H. Nasal carriage of Staphylococcus aureus: epidemiology, underlying mechanisms, and associated risks. Clin Microbiol Rev. 1997;10:505-20. Level I.
4 Pearl TM, Golub JE. New approaches to reduce Staphylococcus aureus nosocomial infection rates: treating S. aureus nasal carriage. Ann Pharmacother. 1998;32:S7-16. Level I.
5 VandenBergh MF, Kluytmans JA, van Hout BA, Maat AP, Seerden RJ, McDonnel J, Verbrugh HA. Cost Effectiveness of perioperative mupirocin nasal ointment in cardiothoracic surgery. Infect Control Hosp Epidemiol. 1996;17:786-92. Level I.
6 Wenzel RP, Perl TM. The Significance of Nasal Carriage of Staphylococcus aureus and the Incidence of Postoperative Wound Infection. Journal of Hospital Infection. 1995;31,13-24. Level I.
7 Ammerlann HS, Kluytmans JA, Wertheim HF, et al. Eradication of Methicillin-Resistant Staphylococcus aureus Carriage: A Systematic Review. Healthcare Epidemiology 2009;48:922-930. Level I.
8 Whitehouse JD, Friedman ND, Kirkland KB, Richardson WJ, Sexton DJ. The impact of surgical-site infections following orthopaedic surgery at a community hospital and a university hospital: adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol. 2002;23: 183-9. Level I.
9 Vonberg RP, Stamm-Balderjahn S, Hansen S, et al. How often do asymptomatic
healthcare workers cause methicillin-resistant Staphylococcus aureus outbreaks? A
systematic evaluation. Infect Control Hosp Epidemiol. 2006;27:1123-1127. Level I.
10 Schwarzkopf R, Takemoto RC, Immerman I, Slover JK, Bosco JA. Prevalance of Staphylococcus Aureus Colonization in Orthopaedic Surgeons and Their Patients: A Prospective Cohort Controlled Study. Journal of Bone and Joint Surgery. August 2010. Level I.
11 Kalmeijer MD, van Nieuwland-Bollen E, Bogaers-Hoffman D, et al. Nasal Carriage of Staphylococcus aureus is a Major Risk Factor for Surgical Site Infections in Orthopaedic Surgery. Infect Control Hosp Epidemiol. 2000;21:319-323. Level I.
12 Bode LG, Kluytmans JA, Wertheim HF, et al. Preventing surgical-site infections in
9 nasal carriers of Staphylococcus aureus. N Engl J Med. 2010 Jan 7;362(1):9-17. Level I.
13 Germaat-van der Sluis AJ, Hoogenboom-Verdegaal AM, Edixhoven PJ, Spies-van Rooijen NH. Prophylactic mupirocin could reduce orthopaedic wound infections. 1,044 patients treated with mupirocin compared with 1,260 historical controls. Acta Orthop Scand. 1998;69:412-4. Level I.
14 Rao N, Cannella B, Crossett LS, Yates AJ Jr, McGough R 3rd. A preoperative decolonization protocol for staphylococcus aureus prevents orthopaedic infections. Clin Orthop Relat Res. 2008;466:1343-8. Level II.
15 Kluytmans JA, Mouton JW, VandenBergh MF, Manders MJ, Maat AP, Wagenvoort JH, Michel MF, Verbrugh HA. Reduction of surgical-site infections in cardiothoracic surgery by elimination of nasal carriage of Staphylococcus aureus. Infect Control Hosp Epidemiol. 1996;17:780-5. Level I.
16 Kluytmans JA, Manders MJ, van Bommel E, Berbrugh H. Elimination of nasal carriage of Staphylococcus aureus in hemodialysis patients. Infect Control Hosp Epidemiol. 1996;17:793-7. Level I.
17 Skeete F, Berger N, Kraemer K, Comeau L, et al. Surgical Site Infection Prevention Initiative: Patient Attitude and Compliance. Association for Professionals in Infection Control and Epidemiology. Washington DC. July 2010. Level I.
18 S. Ridgeway et al., Infection of the surgical site after arthroplasty of the hip, J Bone Joint Surg Br 87-B (2005), p. 844. Level I.
19 C.S. Price, A. Williams and G. Philips et al., Preoperative decolonization protocol for Staphylococcus aureus prevents orthopaedic infections, Clin Orthop Relat Res 466 (2008), p. 2842. Level I.
20 M.D. Kaljmeijer et al., Nasal carriage of Staphylococcus aureus is a major risk factor for surgical site infections in orthopedic surgery, Infect Control and Hosp Epidemiol 21 (2000), p. 319. Level I.
21 M.D. Kaljmeijer et al., Surgical site infections in orthopedic surgery: the effect of mupirocin nasal ointment in a double-blind, randomized, placebo-controlled study, Clin Infect Dis 35 (2002), p. 353. Level I.
22 K.J. Bozic and M.D. Ries, The impact of infection after total hip arthroplasty on hospital and surgeon resource utilization, J Bone Joint Surg Am 87 (2005), p. 1746. Level I.
23 Hacek DM, Robb WJ, Paule SM, Kudrna JC, Stamos VP, Peterson LR. Staphylococcus aureus nasal decolonization in joint replacement surgery reduces infection. Clin Orthop Relat Res 2008;466:1349-1355. Level III.
24 van Rijen MM, Bonten M, Wenzel RP, Kluytmans JA. Intranasal mupirocin for reduction of Staphylococcus aureus infections in surgical patients with nasal carriage: a systematic review. J Antimicrob Chemother 2008;61:254-261 Level I.
25 Tom T, Kruse MW, Reichman R. Update: Methicillin-Resistant Staphylococcus aureus Screening and Decolonization in Cardiac Surgery. Ann Thorac Surg 2009;88:695-702. Level I.
26 Davis KA, Stewart JJ, Crouch HK, Florez E, Hospenthal DR. Methicillin-resistant Staphylococcus aureus (MRSA) nares colonization at hospital admission and its effect on subsequent MRSA infection. Clin Infect Dis 2004;39:776-82. Level I.
27 Levenson D. The path to better MRSA control: how active surveillance and molecular tests can reduce infections and transmission. Clin Lab News 2007;33:1-7. Level I.
28 Albrich EC, Harbarth S. Health-care workers: source, vector, or victim or MRSA? Lancet Infec Dis 2008;8:289-301. Level I.
29 Cesur S, Cokca F. Nasal carriage of methicillin-resistant Staphylococcus aureus among hospital staff and outpatients. Infect Control Hosp Epidemiol 2004;25:169-70. Level I.
30 Blok HEM, Troelstra A, Hamp-Hopmans TEM, et al. Role of healthcare workers in outbreaks of methicillin-resistant Staphylococcus aureus: a 10-year evaluation from a dutch university hospital. Infect Control Hosp Epidemiol 2003;24:679-85. Level I.
31 Bosco JA, Slover JD, Haas JP. Perioperative Strategies for Decreasing Infection. A Comprehensive Evidence-Based Approach. The Journal of Bone and Joint Surgery (American). 2010;92:232-239. Level I.
32 Wenzel RP, Perl TM. The significance of nasal carriage of Staphylococcus aureus and the incidence of postoperative wound infection. J Hosp Infect. 1995;31:13-24. Level I.
33 Perl TM, Cullen JJ, Wenzel RP, Zimmerman MB, Pfaller MA, Sheppard D, Twombley J, French PP, Herwaldt LA; Mupirocin and the Risk of Staphylococcus Aureus Study Team. Intranasal mupirocin to prevent postoperative Staphylococcus aureus infections. N Engl J Med. 2002;346:1871-7. Level I.
34 Kalmeijer MD, van Nieuwland-Bollen E, Bogaers-Hofman D, de Baere GA. Nasal carriage of Staphylococcus aureus is a major risk factor for surgical-site infections in orthopaedic surgery. Infect Control Hosp Epidemiol. 2000;21:319-23. Level I.
35 Harbarth S, Fankhauser C, Schrenzel J, Christenson J, Gervaz P, Bandiera-Clerc C, Renzi G, Vernaz N, Sax H, Pittet D. Universal screening for methicillin-resistant Staphylococcus aureus at hospital admission and nosocomial infection in surgical patients. JAMA. 2008;299:1149-57. Level I. |