Address for Correspondence
Prince of Wales Hospital, Suite 29 Level 7, Barker Street, Randwick. NSW 2031. Australia.
Phone: +61 2 9650 4397
Fax: +61 2 9650 4905
Email: jonathanmulford@myorthopod.com.au
Website: myorthopod.com.au
Abstract
Background: A case history of a sarcoma abutting a unicompartmental knee replacement is presented with a review of the literature on knee arthroplasty and associated malignancy.
Literature: There are 25 cases described in the literature with only 3 reports demonstrating an association with knee arthroplasty. Data linking joint replacement and subsequent malignancy is controversial and scarce. The available data at present does not support a link between arthroplasty and the development of malignancy.
Clinical Relevance: An association between arthroplasty and malignancy was raised with our case history. The case contributes to the available literature and provides a review of the literature.
Case Report
A 91year old male presented to our institution 15 months after he began to develop swelling and ulceration in close proximity to a previous left medial unicompartmental knee arthroplasty performed 15 years previously. There was no history of previous problems with the implant and no previous history of malignancy or any notable family history. He resided in a nursing home and had moderate dementia.
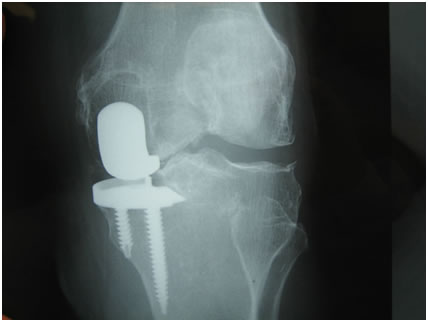
The patient was apyrexial with no systemic signs of sepsis. He had a mass on the medial aspect of his left knee with a 1.5cms x 2cms area of ulceration over a fungating mass at the most prominent part of the swelling. (Figure 1 ). He had anaemia (Haemaglobin 59) of chronic disease and a white cell count of 15. X-rays demonstrated a unicompartmental knee prosthesis with no obvious complication around the components (fig 2).
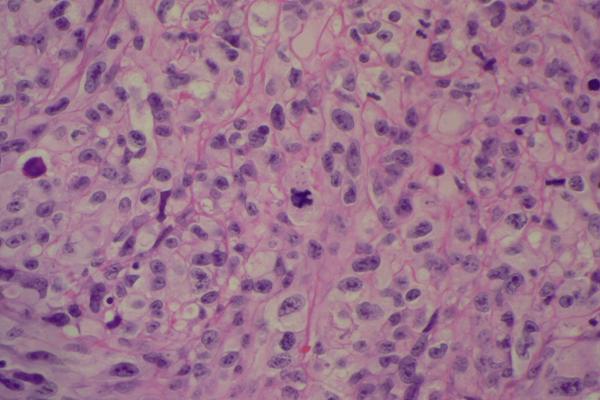
The patient had a washout and biopsy of the lesion. Microbiology culture confirmed colonisation with pseudomonas. The microscopic histological appearance was of a high grade grade sarcoma, probably a malignant fibrous histiocytoma. The malignancy was undifferentiated on morphology and on immunoperoxidase staining. Further evaluation was performed and the case was discussed at a regional bone tumour meeting concluding a high grade myxofibrosarcoma. (Fig. 3)
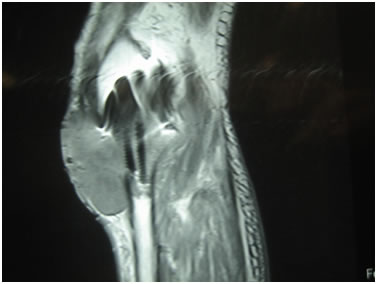
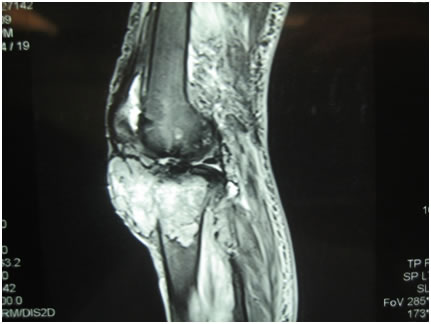
MRI of the knee showed a large, low density mass in the metaphyseal region of the upper tibia intimately associated with the prosthesis. The mass had eroded through the anterior cortex of the tibia and extended to the joint surface and 45mm into the suprapatella pouch. The femur was not involved. (Fig 4 and 5).
Access to the original pre and postoperative images of the arthroplasty was not available. Discussions with the patient and family revealed the patient had been asymptomatic since the insertion of the prosthesis. We concluded from this that there was no pre-existing lesion at the time of implantation. Discussion was initiated with the family regarding amputation but was declined. The patient was discharged back to the nursing home and has not returned for follow up.
J.Orthopaedics 2011;8(3)e6

F(1)
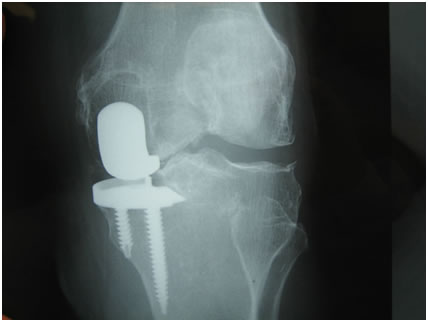
F(2)
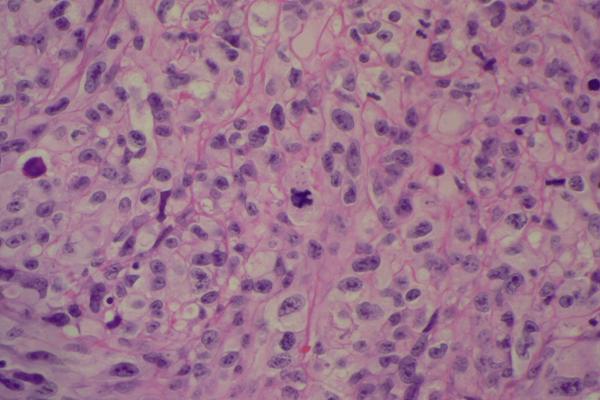
F(3)
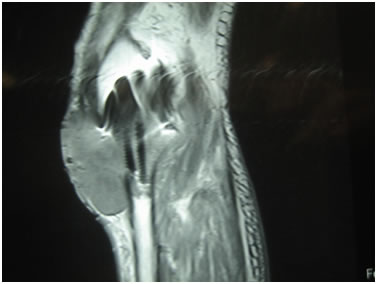
F(4)
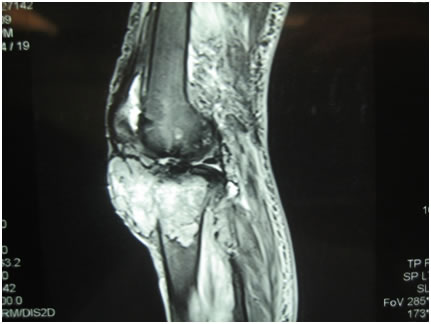
F(5)
Discussion :
The MRI findings of the tumour abutting the joint replacement raised the question, “does the implant have a aetiological role in the manifestation of the tumour?” With the incidence of knee arthroplasty rising and being utilised in younger patients this is of concern. The literature was thus reviewed.
The Regional Bone Tumour Multidisciplinary Meeting consensus was that the prosthesis was probably the cause of the tumour, however, a definite causal relationship was difficult to prove. The conclusion was based on the fact that malignancy at other sites had been excluded, no abnormality of the bone prior to arthroplasty existed, no known risk factors for malignancy (e.g. Paget’s disease, haemopoietic cancer and steroid use), radiological examination revealed an intimate association of the tumour with the prosthesis and histological examination revealed no evidence of a primary tumour at a remote site. Ideally histopathological examination of the specimen should reveal intimate association of the tumour with the prosthesis.
There are theoretical reasons why sarcoma may develop at the site of arthroplasty. Surgery or poly methyl methacrylate (PMMA) may induce osteonecrosis which is a precursor to the development of tumours, in particular, malignant fibrous histiocytoma (MFH). This has been reported in association with hip arthroplasty ( 2, 3, 9, 10, 14,). Metal debris generated by the implants themselves has been implicated in carcinogenesis as has polyethylene debris largely in hip arthroplasty with metal on metal bearings (5, 20, 21, 22, 23). Metal ions are not of concern for knee replacement surgery. Underlying Paget’s disease, haemopoietic malignancies, undiagnosed tumours and steroid therapy have been implicated in the development of MFH (12). Occult sarcomas have been missed in patients undergoing total hip arthroplasty (2).
Literature review revealed twenty five case reports of malignancy in association with arthroplasty. Of these, only three related to knee arthroplasty with the remainder being associated with hip arthroplasty(17) (15) (16). All these three cases were sarcoma type lesions. There is therefore scarce anecdotal evidence of knee arthroplasty increasing the risk for malignancy.
There have been previous reviews looking for associations between arthroplasty and malignancy (5) (6) (13) (24) (8). The overwhelming conclusion from these reviews is that the available data does not support a link between hip or knee arthroplasty and the development of cancer. If there is any association it has been estimated the risk of an osteosarcoma developing after a THA is estimated to be 12 per million implants per year (3). The risk of developing an osteosarcoma from background radiation alone is 20 per million.
Conclusion
Periprosthetic tumour is rare with insufficient evidence at present to link arthroplasty to the development of malignancy. If there is an association it is rare. Only reporting of such possible arthroplasty related tumours will reveal any association.
Reference :
- Vigorita VJ. Orthopaedic Pathology second edition (2008). Lippincott Williams and Wilkins. Philadelphia, PA 19106 USA. LWW.com
- Bago-Granell J, AguirreCanyadell M, Nardi J, Tallada N. Malignant fibrous histiocytoma of bone at the site of a total hip arthroplasty. JBJS (Br):1984. Vol 66-B: 38-40
- Galante JO, Lemons J, Spector M. The biologic effects of implant materials. J Orthopaedic Research 1991: 9; 760-775
- Sirveaux F, Hummer N, Roche O, Rios M, Vignaud JM, Mole D. Pleaomorphic malignant fibrous histiocytoma at the site of an arthroscopic reconstruction of the anterior cruciate ligament. A Case Report. JBJS 2005: 87A; 404 – 409
- Daley B, Dohery AT, Fairman B, Case CP. Wear debris from hip or knee replacements causes chromosomal damage in human cells in tissue culture. JBJS(Br) 2004;86; 598 -606
- Davies AP, Sood A, Lewis AC, Newson R, Learmonth ID, Case CP. Metal-Specific differences in levels of DNA damage caused by synovial fluid recovered at revision arthroplasty. JBJS(Br) 2005 : 87; 1439 – 1444
- Cheuk W, Chan ACL, Chan JKC. Metallic Implant-associated lymphoma. A distinct group of large B-Cell lymphoma related to pyothorax associated lymphoma? Am J Surg Path 2005 :29 (6); 832 – 836
- Tharani R, Dorey FJ, Schmalzried TP. The Risk of Cancer Following Total Hip or Knee Arthroplasty. JBJS (Am) 2001;83:774-780
- Swann M. Malignant Soft-tissue Tumour at the site of a Total Hip Replacement. JBJS (Br) 1984; 66-B; 5:629-631
- Martin A, Bauer TW, Manley MT, Marks KE. Osteosarcoma at the site of Total Hip Replacement. JBJS Am 1998;70:1561-1567
- Penman HG, Ring PA. Osteosarcoma in association with Total Hip Replacement. JBJS(Br)1984; 66;5:632-634
- Solomon MI, Sekel RS. Total Hip Arthroplasty complicated by a malignant fibrous histiocytoma. A case report. J.Arthroplasty. 1992;7:549-550
- Lewold S, Olsson H, Gustafson P, and Rydholm AR, Lidgren L. Overall Cancer Incidence Not increased after prosthetic knee replacement: 14,551 patients followed for 66,622 patient years. Int. J. Cancer. 68, 30-33 (1996)
- Hamblen DL. Sarcoma and Joint replacement. JBJS (Br). Vol 66-B,No5:Nov 1984: 625-627
- Weber PC. Epithloid Sarcoma in association with total knee replacement. JBJS(Br) 1986 ;68:824-826
- Eckstein FS, Vogel U, Mohr W. Fibro sarcoma in association with a total knee joint prosthesis. Virchow’s Archiv A Pathol Anat (1992) 421: 175-178
- Iglesias ME, Vazquez Doval FJ, Idoate F, Valenti JR, Quintanilla E. Malignant Fibrous histiocytoma at the site of total knee replacement. J dermatol surg oncol. 1994;20:848-9
- Cole BJ, Schulz E, Smilari TF, Hajdu SI, Krauss ES. Malignant fibrous histiocytoma at the site of a total hip replacement: review of the literature and case report. Skeletal radiology 1997 Sept. 26(9):559-63
- Coleman RF, Herrington J, Scales JT. Concentration of wear particles in hair, blood and urine after total hip replacement. BMJ 1973:1;527-529
- Ferguson AB, Laing PG, Hodge ES. The ionisation of metal implants in living tissues. JBJS: 1960: 42(A);77-90
- Heath JC, Freeman MAR, Swanson SAV. Carcinogenic properties of wear particles from prostheses made in cobalt-chromium alloy. Lancet: 1971:1 564-566
- Siddons AHM, Macarthur AM. Carcinomata developing at the site of foreign bodies of the lung. Br J Surg 1952: 39: 542-545
- Swanson SAV, Freeman MAR, Heath JC. Laboratory tests on total joint replacement prostheses. JBJS(Br) 1973: 55-B(4):759-773
- Dennis DA. Alternative Bearings in Total Hip Arthroplasty. Instructional Course Lecture. Course 153. American Academy of Orthopaedic Surgeons Annual Meeting 2010. New Orleans. USA.
|