Address for Correspondence
Jimenez ,University of Castilla and la Mancha Toledo, Spain
Email:josefernando.jimenez@uclm.es
Abstract:
AIM: to describe the efficacy of sonography (ultrasound) in the diagnosis of chronic muscular lesions and in the prevention of the risk of recurrence in the injured muscle by using dynamic ultrasound and electromyographic examination during static and dynamic strength exercises.
CONCLUSIONS: The use of ultrasound and electromyography to dynamically evaluate the bioelectrical and morphological profile of muscle while performing exercises similar to those which provoked an injury has proved efficient.
J.Orthopaedics 2011;8(2)e2
Key words: dynamic ultrasound, electromyography, muscular lesion
Introduction
In recent years, sonography has become a very useful tool in the study of locomotor system injuries, particularly in soft tissues, because it is here that muscle overloading pathologies usually occur (1).
With the development of new techniques used in sonography, such as tissue harmonic imaging, side-view imaging or compound techniques, panoramic examination or 3D study (2, 3), together with the use of high-frequency probes, ultrasonography has become an ever more useful tool to evaluate musculoskeletal injuries (4). This state-of-the-art equipment permits the evaluation of the slightest injuries with a high degree of sensitivity (5). This equipment has a great number of advantages including portability and relatively low cost. The possibility of implementing dynamic studies when examining muscle injuries allows accurate diagnosis of minor injuries which might otherwise remain undetected when the structures involved are not in movement. These examinations are usually carried out by performing isometric contractions and muscle relaxations. In other cases, the dynamic study involves the execution of active or passive articular movements with displacement of the soft tissues concerned.
Muscle ultrasound anatomt
Muscles are surrounded by a 3-layer dense connective tissue (6, 7). The outermost layer, the epimysium, is very echogenic and extends towards the inner part of the muscle until it reaches the perimysium or fibroadipose septum, which is also very echoic and contains connective tissue, fat, vessels and nerves, and divides the fascicle into muscle fibers. Muscle fibers are formed by myofilaments surrounded by a connective tissue web, the endomysium, which contains capillaries and nerves. The endomysium, however, cannot be visualized with ultrasound (8). Fibers are arranged either linearly or obliquely until they reach the myotendinous junction (MTJ), an extremely vulnerable area of variable size (in some cases it can be larger than half the muscle length). br> For a better understanding of the clinical case described here, we must remember that the hamstrings are inserted into the tuber ischiadicum. A longitudinal ultrasound examination clearly reveals the insertion of the semitendinosus muscle (medial area), of the semimembranosus muscle (lateral area) and of the large portion of the biceps femoris (lateral and posterior area). There is a characteristic fiber pattern in all of them and it is important to note the occurrence of anisotropy. A transverse study reveals how the MTJ are arranged in the insertion area.
A CLINICAL CASE OF DISRUPTION OF THE MYOTENDINOUS JUNCTION OF BICEPS FEMORIS
During strenuous muscle stretching exercises, the muscles undergo strong traction forces which overload the muscle fibrils and occasionally provoke a rupture near the MTJ (9). This kind of muscle strain normally affects the superficial muscles which work in two articulations. This is the case of the rectus femoris, the semitendinous muscle, the biceps femoris and the gastrocnemius muscles (10, 11, 12).
Biceps femoris has two heads. The long head originates in the medial facet of ischial tuberosity via a tendon shared with the semitendinosus muscle, whereas the short head emerges from the femur linea aspera. It is distally attached to the tibia lateral condyle and more distally to the fibula head (13, 14).
The subject of our study was a 28-year old, 191 cm tall, professional basketball player weighing 95 kg. Five months earlier the player had suffered an indirect-type acute muscle fiber injury (15, 16) in the biceps femoris muscle of his right thigh. After five days of inactivity, the player resumed his training program with some slight pain. Eventually, 30 days later, the injury recurred showing a clinical picture of intense pain and complete functional disability for walking. For this reason, the player received echo-guided treatment with platelet factors and physiotherapy. Finally, the player followed a functional rehabilitation program until he could rejoin the competition five weeks after the recurrence.
The player was able to compete under those conditions for the remaining two months of competition, playing on average two to three matches per week. However, slight pain in the injured area, particularly in knee-bending or hip-extending movements, to some extent prevented him from adequately performing some of the very demanding exercises on the court.
Injury ulrtasound examination
As a result, at the end of the official competition five months after the first injury, the player underwent an ultrasound examination by means of transverse and longitudinal sections in the posterior side of the right thigh. The potential of this sonography led us to carry out a bilateral study (17, 18) of the posterior side of the upper third of the thigh in order to examine the proximal MTJ of biceps femoris. The test revealed a hypoechoic surface with the typical tuft pattern of the muscle (19) in complete disarray but surrounded by normal muscle tissue (20). The image was situated very near the sciatic nerve trajectory (Fig. 1). The transverse study also revealed a triangular hypoechoic area which, in close connection with this nerve (Fig. 2 and 3), provoked referred pain. Although no blood collections or calcifications were found, the Power Doppler revealed (21, 22) few vessels, the result of the long-term character of the injury (Fig. 4). Finally, with a powerful 3D study (23, 24) projected onto a number of volumetric cubes, the evaluation of the axial and sagittal planes allowed a tomographical analysis of the injured area (Fig. 5). All these images confirmed the diagnosis: an early-stage fibrous scar (25) in the right biceps femoris muscle at the proximal muscle-tendinous junction.
At the end of a 12-week progressive program of physical exercises, a new ultrasound examination checked the state of the injury at the proximal MTJ of the biceps femoris. The examination revealed a heteroechoic area corresponding to regeneration tissue in the area near the sciatic nerve (Fig. 6). As compared with the previous ultrasound image, the injured area had been filled in (Fig. 7) and new fibers were visible. The Power Doppler revealed no vascularization, which proved that the regenerative process had terminated. These images confirmed the ultrasound diagnosis of fibrous regeneration of the right biceps femoris muscle at the proximal MTJ, in an area adjoining the sciatic nerve.
COMPLEMENTARY EVALUATION STUDIES OF THE FUNCTION OF THE INJURED MUSCLE
There are several methods available for the diagnosis of a muscular lesion (26). In order to design a well-planned recovery program of appropriate training, our work concentrated on the muscle's functional response in relation to force (27, 28). For this purpose we examined the electromyographic (EMG) and sonodynamic (21) behaviour of the muscle, since this allows us to study and determine the profile of an injured biceps femoris muscle (29) during the course of a static and dynamic strength exercise program (Fig. 8) (30).
Using a fastening system we attached EMG electrodes (as recommended by SENIAM) (31) and an ultrasound probe to the posterior side of the thigh at the level of the injured area previously identified by ultrasound examination. The athlete warmed up for 5-10 minutes in a tempo run at the speed and slope that he himself deemed most appropriate. Tests were carried out as described below.. All tests were first performed on only one leg (first the right leg and then the left leg) and subsequently on both legs.
1-. Isometric contraction of hamstrings: in prone decubitus position the athlete brought the axis of his knee in line with that of the machine and the lower roller was placed on the median third of his Achilles' tendon. On hearing the signal he bent his knee 90° with the isometric contraction (the machine was adapted to limit the movement). He performed a maximum contraction for 5 seconds (with his hip attached to the machine to prevent the action of the erector spinae muscles). We recorded force (N) and relative power (W/kg).
2-. Dynamic force evaluation in the performance of two different vertical jumps frequently used for this purpose at different ages, from children (32, 33), to adolescents and adults (34):
2.1. Squat Jump - SJ : the athlete performed a vertical jump from a half-squat position (knee bent 90°), with the trunk upright and his hands on his hip. The subject performed the test without any previous counter-movement.
2.2. Counter Movement Jump – CMJ: in upright position with his hands on his hip, the subject made a vertical jump with a previous counter-movement (his knees bent in any position).
With these tests we reckoned the jump height (cm) from the flight time (35) and the force (N and %bw) and relative power values (W/kg) during take-off and landing. In addition, via EMG the electrical activity values were analysed and dynamic ultrasound enabled us to measure muscle thickness by measuring the distance between aponeurosis (29).
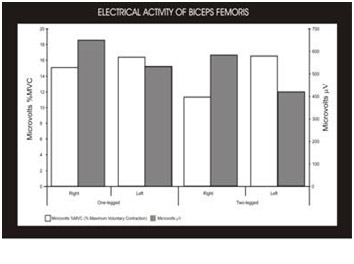
Muscle electrical activity taken during the isometric test revealed higher mean values in the right biceps, as expected in a dominant limb. However, the peak values of electrical activity in the right biceps were lower as a result of the fibrous fiber injury (Fig. 9).
The dynamic force value reached higher bioelectrical activity in the left biceps muscle than in the right biceps muscle at maximum power point during the two-leg SJ. Dynamic force records during the two-legged CMJ jump also presented higher bioelectrical activity in the left biceps muscle at the maximum power point (Fig. 10). These data revealed a clear functional deficit in the right biceps as a result of the fiber injury.
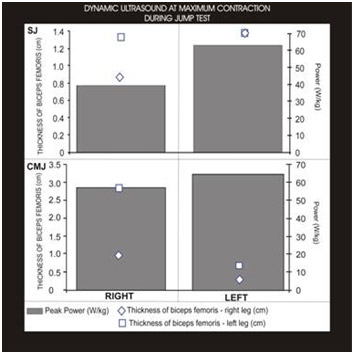
Finally, the dynamic ultrasound data recorded during the isometric contraction test revealed that the right biceps femoris had greater muscle fiber thickness than the left biceps at the moment of maximum contraction, both in the one-leg test and in the two-leg test (Fig. 11).
Conclusion
1-. Ultrasound techniques have proved to be an extremely useful tool in the examination of chronic muscle injuries with delayed fiber scar formation.
2-. Ultrasound can play a significant role in the detailed examination of the development of scar injuries in high-performance athletes, since it permits accurate evaluation of the healing phase of disrupted muscles.
3-. The simultaneous recording of ultrasound data and electromyographic data during the performance of exercises testing the functionality of an injured muscle opens up a new field in the functional evaluation of injured muscles.
4-. The isometric tests revealed higher mean values in the bioelectrical activity of the right biceps, which is to be expected in a dominant limb. However the peak values of the electrical activity in the right biceps were lower. This was probably due to the fiber injury.
5-. The analysis of the dynamic force values revealed higher bioelectrical activity in the left biceps muscle than in the right one at maximum power point during the two-legged SJ and CMJ jumps. This was most likely related to the injury in the right biceps femoris.
6-. Finally, the dynamic ultrasound examination carried out during the isometric test revealed greater thickness of the right biceps femoris muscle compared to the contralateral biceps. Nevertheless, the muscle function remains within relatively normal records and the rehabilitation program could therefore begin.
FIGURES
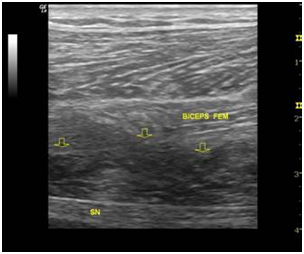
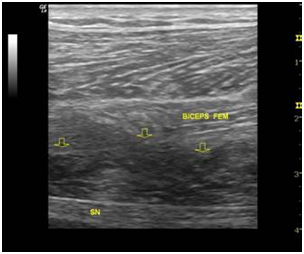
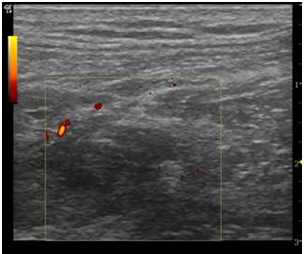
Fig. 1- The longitudinal examination of the posterior side of the thigh 5 months after the occurrence of the injury reveals a hypoechogenic area (arrows) in the deep portion of the biceps femoris muscle above the sciatic nerve (SN).
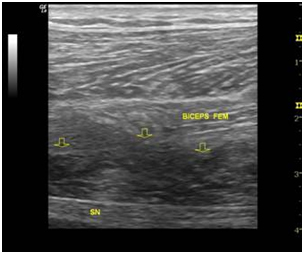
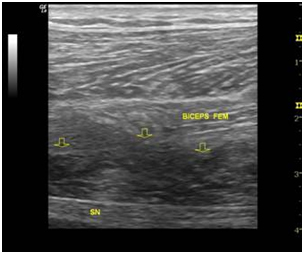
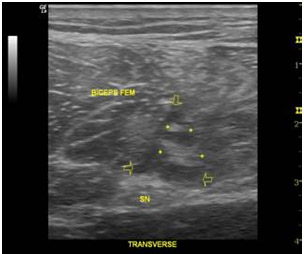
Fig. 2- This transverse examination reveals, in the deep plane of the biceps muscle, a triangular hypoechogenic area (arrows) which corresponds to the scar area and is surrounded by normal muscle tissue.
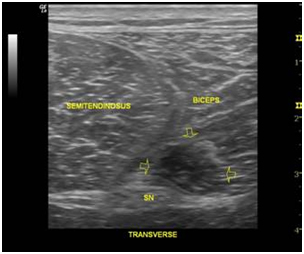
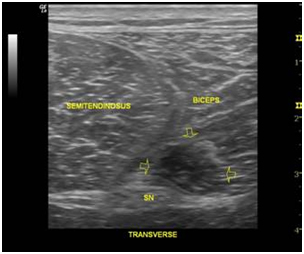
Fig. 3- This comparative view reveals a hypoechogenic area (right side of the image) which disrupts the normal muscle pattern.
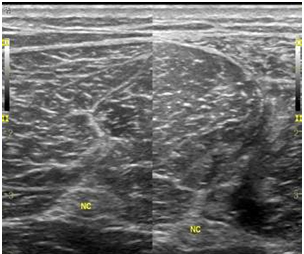
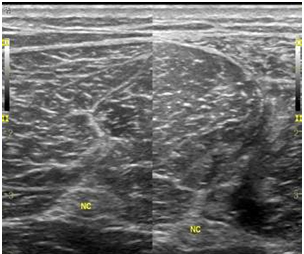
Fig. 4- The application of Power Doppler in this longitudinal section reveals few vessels in the scar area.
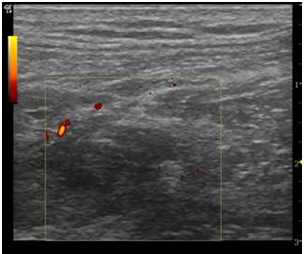
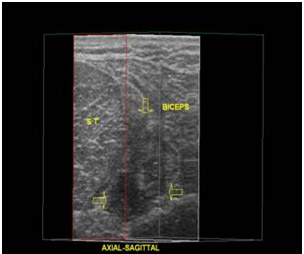
Fig. 5- A 3D examination permits the tomographical evaluation of the injured area.
This axial-sagittal section reveals the depth of the hypoechogenic area (arrows), between the femoral biceps and the semitendinosus muscle (ST).
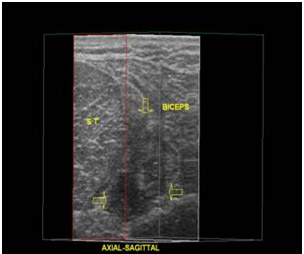
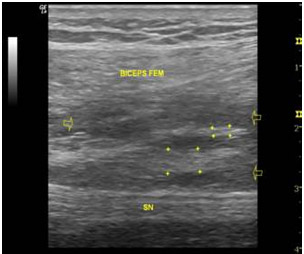
Fig. 6- The longitudinal examination carried out 7 months after the injury reveals the fibrous regeneration area (+) on the scar injury area. Small hypoechogenic areas still persist.
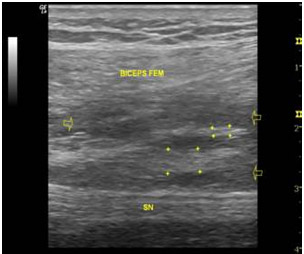
Fig. 7- The transverse examination reveals that the hypoechoic triangle is filled with fiber areas (+) and some poorly reflectant areas (arrows) above the sciatic nerve (SN).
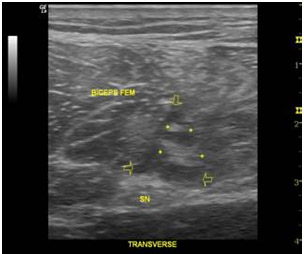
Fig. 8- The player is on the force platform. Dynamic ultrasound data and biolectrical activity data are recorded simultaneously by means of electromyographic probes.

Fig. 9- Maximum electromyographic values (microvolts) and mean values (% of maximum) for the femoral biceps in the isometric test.
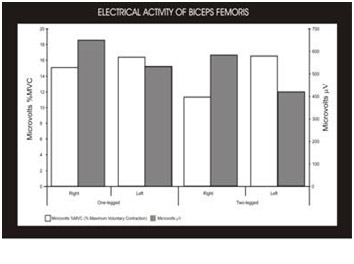
Fig. 10- Dynamic ultrasound values (muscle thickness) of the femoral biceps at the maximum power point during CMJ and SJ jumps
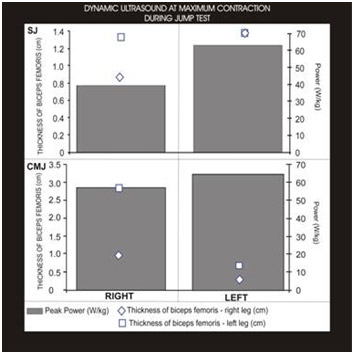
Fig. 11- The isometric contraction test to reckon the muscle thickness reveals normal behaviour of the right femoral biceps

References
- Jiménez F, Villa G, García A, González M. Rodilla de saltador en jugador de basket. Arch Med Dep. 2007; XXIV(2):118:215-216.
- Barberie J, Wong A, Cooperberg P, Carson BW. Extended Field-of-View Sonography in Musculoskeletal Disorders. AJR.1998; 171:751-757.
- Jiménez JF, Alvarez G, Balius R, Berral FJ, Lara E. New Technologies applied to Ultrasound Diagnosis of Sports Injuries. Adv Ther 2008; 25(12): 1315-1330.
- Chun Koh ES, McNally EG. Ultrasound of Skeletal Muscle Injury. Semin Musculoskelet Radiol. 2007; 11:162-173.
- Koulouris G, Connell D. Hamstring muscle complex: an imaging review. Radiographics. 2005; 25(3):571–586.
- Takala TE, Virtanen P. Biochemical composition of muscle extracellular matrix: the effect of loading. Scand J Med Sci Sports. 2000; 10:321-325.
- Peetrons P. Ultrasound of muscles. Eur Radiol. 2002; 12:35-43.
- Jiménez F. Ecografía del aparato locomotor. Ed. Marbán. Madrid. 2007.
- Jarvinen TA, Järvinen TLN, Kääriäinen M, Kalimo H, Järvinen M. Muscle injuries: biology and treatment. Am J Sports Med. 2005; 33(5):745-764.
- Garrett WE. Muscle strain injuries. Am J Sports Med. 1996; 24:S2-S8.
- Kalimo H, Rantanen J, Järvinen M. Muscle injuries in sports. Baillieres Clin Orthop. 1997; 2:1-24.
- Kujala UM, Orava S, Järvinen M. Hamstring injuries: current trends in treatment and prevention. Sports Med. 1997; 23:397-404.
- Koulouris G, Connell D. Hamstring muscle complex: an imaging review. Radiographics. 2005; 25(3):571–586.
- Standring S. The anatomical basis of clinical practice. Gray’s Anatomy. 39th ed. Edinburgh, UK: Churchill Livingstone; 2004.
- Vlychou M, Teh J. Ultrasound of muscle. Curr Probl Diagn Radiol. 2008;37:219-230.
- Muñoz, S. Lesiones musculares deportivas: diagnóstico por imágenes. Rev Chil Radiol. 2002; 8:127-132.
- Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease: a comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006; 88:1699–1704.
- Levin D, Nazarian LN, Miller TT, et al. Sonographic detection of lateral epicondylitis of the elbow. Radiol. 2005; 237:230–234.
- Fornage BD, Nerot C. Sonographic diagnosis of rhabdomyolysis. J Clin Ultrasound .1986; 14:389-392.
- Fornage BD. The case for ultrasound of muscles and tendons. Semin Musculoskelet Radiol. 2000; 4:375-391.
- Nazarian L. The top 10 reasons musculoskeletal sonography is an important complementary or alternative technique to MRI. AJR. 2008; 190:1621-1626
- Zanetti M, Metzdorf A, Kundert HP, et al. Achilles tendons: clinical relevance of neovascularization diagnosed with power Doppler US. Radiol. 2003; 227:556–560.
- Jiménez F, Barriga A, López J. Aplicación de la ecografía tridimensional en el diagnóstico de las lesiones músculo-esqueléticas. Arch Med Dep. 2007; XXIV(2) 118:103-111.
- .
- Jiménez F, Mendizábal S, Rubio JA. Utility of the 3 dimensions ultrasound scan in the study of the tendons ruptures. Arch Med Dep. 2008; XXV(6)128:546.
- Balius R, Rius M, Combalia A. “Ecografía muscular de la extremidad inferior”. Ed. Masson. Barcelona. 2005.
- Rodas JA, Insunza A, Del Valle M. Muscular injuries diagnosed by ultrasound and blood analysis in football players. Arch Med Dep. 2008; XXV(6)128:546.
- Brorsson S, Nilsdotter A, Hilliges M, Sollerman C, Ylva A. Ultrasound evaluation in combination with finger extension force measurements of the forearm musculus extensor digitorum communis in healthy subjects. BMC Med Imaging. 2008;8(6):1-10.
- Bojsen-Moller J, Hansen P, Aagaard P, Kjaer M, Magnusson SP. Measuring mechanical properties of the vastus lateralis tendon-aponeurosis complex in vivo by ultrasound imaging. Scand J Med Sci Sports. 2003;13(4):259-265.
- Chleboun GS, France AR, Crill MT, Braddock HK, Howell JN. In vivo measurement of fascicle length and pennatin angle of the human biceps femoris muscle. Cells Tissues Organs. 2001;169:401-409.
- Lieber LR, Frdén J. Functional and clinical significance of skeletal muscle architecture. Muscle Nerve. 2000; 23(11):1647-1666.
- Hermens HJ, Merletti R, Freriks B. European Recommendations for Surface Electromyography. Results of the SENIAM project. 3nd ed. 1999:SENIAM.
- Rubio JA, Abián J, Alegre LM, Lara AJ, Miranda A, Aguado X. Capacidad de salto y amortiguación en escolares de primaria. Arch Med Dep. 2007;XXIV(120):235-244.
- McKay H, Tsang G, Heinonen A, MacKelvie K, Sanderson D, Khan KM. Ground reaction forces associated with an effective elementary school based jumping intervention. Br J Sports Med. 2005;39(1):10-14..
- Ivey FM, Tracy BL, Lemmer JT, et al. Effects of strength training and detraining on muscle quality: age and gender comparisons. J Gerontol A Biol Sci Med Sci. 2000;55(3):B152-157; discussion B158-159
- Linthorne NP. Analysis of standing vertical jumps using a force platform. Am J Phys. 2001;69(11):1198-1204.
|