|
Abstract:
Backround: In recent years, regional anesthesia becomes more common in practise by development of nerve block technics. Regional anesthetic applications like cervical or interscalene brachial plexus blocks are safe and useful alternatives to general anesthesia. The aim of the study is to compare the effectiveness of two different regional anesthesia techniques during orthopaedic shoulder and neck surgery.
Methods: In a prospective study, 60 male patients were randomized into two groups. Group I (DCP; Deep cervical plexus block; n=30) and group II (SC/IBP; Superficial cervical and interscalene brachial plexus block; no=30). All patients received 30 ml 0,5% bupivacaine for regional block. The surgical indications of the groups were mainly similar (torticolis, clavicula fractures, rotator cuff disease, torticollis etc). Motor and sensory blocks, vital measurements (heart rate, blood pressure, O2 -CO2 tension) were being assessed during the procedure. Pain scores and analgesic requirements were evaluated with visual analog scale.
Results: Sensory block was matured in 15-20 minutes and motor block in 20-25 minutes. Pain score assessment of blocks for groups was 3.45-3.11 respectively. No significant differences of vital measurements were noted. Qualitative assessment of blocks was determined as group 1: excellent 24, good 3, except 3 and group 2: excellent 28, good 2. Six patients required additional analgesia at the site of surgery in group I. Neither anesthetic nor surgical complications were observed.
Conclusions: We concluded that, both of classic deep cervical block and combined single injection superficial cervical/interscalene plexus block equally effective. Combined block has slight advantages such as simple and quick application technique, reduced opioid requirements during anesthesia, wide anesthesia exposure (arm and elbow). We believe that both techniques are suitable alternatives to general anesthesia for shoulder girdle and especially in the surgical procedures which are more proximal to shoulder joint
J.Orthopaedics 2011;8(1)e15
Keywords: Shoulder; regional nerve blocks; anesthesia
Introduction
Cervical plexus and interscalene brachial plexus blocks are widely used protocols for many disciplines of contemporary medicine.1,2,3 Increased interest in the use of the cervical plexus block have been popularized for recent years especially in vascular surgery at the neck region.4 Otherwise interscalene brachial plexus block is a well documented and accepted protocol in orthopaedic surgery whereas cervical plexus block is not familiar for orthopaedic surgeons at all.1,2,5
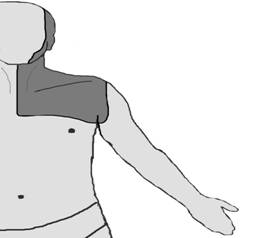
Cervical plexus is formed by the anterior divisions of the four upper cervical nerves and lies in posterior aspect of sternocleidomastoideus muscle with its two main; superficial and deep branches. The branches of the superficial cervical plexus supply innervations to the skin and superficial structures of the head (ante and retro auricular areas) and anterolateral neck.(Figure 1)
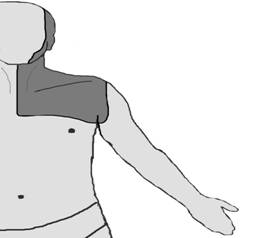
Figure 1
Figure 1: Diagram of the superficial cervical block effect zone.
The deep branches of the cervical plexus innervate the deeper structures of the neck and shoulder, including the muscles (infrahyoid muscles, sternocleidomastoideus muscle, m longus collii, m longus capitis) of this area.6,7 Deep cervical plexus block provides motor and sensory block of the mentioned areas. The sensory component of the cervical plexus can be blocked separately and easily by a superficial cervical block.8,9
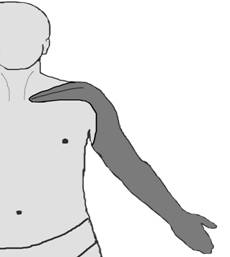
Brachial plexus are formed by anterior roots of fifth cervical- first thoracic spinal nerves with occasional contributions from fourth cervical - second thoracic nerves. Brachial plexus innervates most of the shoulder girdle muscles and remaining distal part of upper extremity. Sensory distribution of brachial plexus begins around the shoulder, girdle through arm except axillary fossa motor and sensory block to the shoulder girdle and upper extremity distal to shoulder joint.8 (Figure2)
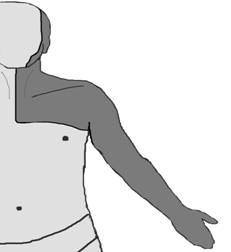
For the purpose of complete anesthesia from neck and clavicular region through the shoulder girdle can be restored by deep cervical block. Combined usage of superficial cervical block/ interscalene brachial plexus block provides a very large anesthesia area from neck to hand. (Figure 3) The purpose of the current study is to demonstrate feasibility of these techniques in upper extremity surgery in orthopaedics and compare the effects of each other.
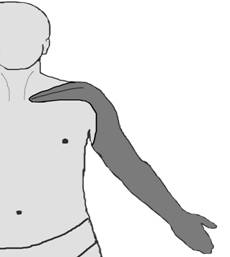
Figure 2 Figure 3
Figure 2: Diagram of the interscallene block effect zone.
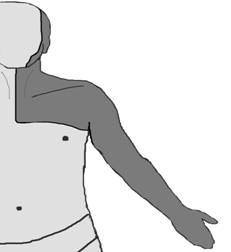
Figure 3: Diagram of the combined superficial cervical / interscalene block effect zone.
Materials and Methods
Sixty male patients who were undergoing orthopaedic surgery around the shoulder girdle for various pathologies were prospectively enrolled in the study and randomised into two groups. Basic parameters of patients were: Age 20 to 26 (mean 23.22 group I, 22.33 group II) years, body weight ranged from 61 to 89 kg (mean weight 67.8 group I, 68.11 group II), all patients were in ASA (American Society of Anesthesiologists) class 1. Obese (body mass index > 30kg/m2) and patients that have cardiac, metabolic or endocrine disorders were excluded. Group I received deep cervical plexus block (DCP n=30) and group II received combination of superficial cervical and interscalene brachial plexus block (SC/IBP no=30). For regional block 30 ml 0,5% bupivacaine was used. All patients were informed of the nature of the study and provided written informed consent. Premedication was not provided in both groups.
Anesthesia Technique
On group 1: Briefly the tip of the mastoid process of the temporal bone, the anterior tubercule on the transverse process of the sixth cervical vertebra (Chassaignac’s tubercle) are located and a straight line is drawn between two tubercule. Approximately 1.5 cm below and 0.6 cm posterior the tip of the mastoid process is marked as first point. Thereafter the third and fourth transverse processes are marked. Landmarks are checked again by locating the sixth transvers process in a cephalad direction.8 Neck is a highly vascular area of the body and needle may be inserted to the area. The needle should be inclined slightly caudad to avoid subarachnoid injections. Also needle is aspirated to avoid intravascular injections. While placing the point of the needle on the tip of the transverse process, the syringe should not be attached to the needle and the needle should be observed for pulsations. After the needle was checked, 10 ml anesthetic solution was injected slowly on each landmark in total of 30 ml.
On group 2: Solution in the subcutaneous space behind the posterior border of the sternocleidomastoid muscle. After that, interscalene brachial plexus block was administered with 20 ml local anesthetic solution while injecting on the lateral border of the anterior scalenus muscle to the anterior border of the medial scalenus muscle.8
Surgical procedures
The types of performed operations in two groups were: group 1 clavicula/neck pathologies (torticolis, clavicula fractures) 15 patients, and shoulder girdle pathologies (proximal humerus fractures, acromyoclavicular separation, bankart lesions, soft tissue tumours, soft tissue contractures etc) 15 patients, group 2 clavicula/neck pathologies 12 patients, and shoulder girdle pathologies 18 patients were underwent surgical intervention. (Table 1) Surgery was performed 20-27 (mean 23.2) minutes after administration of anesthesia.
Table 1
Surgical indications Group I (n= 30 ) Group II ( n = 30 ) |
Torticolis |
7 |
7 |
Clavicular fractures |
8 |
5 |
Acromyoclavicular joint lesions |
7 |
3 |
Proximal humerus fractures |
3 |
6 |
Glenoid cavity fractures |
- |
1 |
Rotator cuff repair |
2 |
1 |
Soft tissue contractures |
1 |
3 |
Anterior capsular tear (bankart lesion) |
- |
2 |
Soft tissue tumours |
2 |
2 |
Table 1: The diagnosis of the patients whom underwent surgery in two groups.
Evaluation methods
Patients were monitored using the Anesthesia Monitor (Narkotron, Generra Medikal, USA) to determine heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), end-tidal carbondioxide and arterial oxygen saturation per operatively.
Motor block was evaluated by quantification of movement at the neck (function of sternocleidomastiod muscle), wrist, elbow and shoulder, according to a rating scale from 5 (full movement) to 0 (no movement). Sensory block was evaluated by testing response to a pinprick in the associated innervation areas. Finally the duration of the sensory and motor block was recorded. Pain scores and analgesic requirements were assessed by VAS (visual analog scale 0-10) at every 15 minutes intraoperative period and postoperative period for 24 hours. Patients were followed up three days postoperatively.
Statistical Analysis
Assessment of data for statistical analysis SPSS (statistical package for social sciences) for windows was used. Evaluate the data; either descriptive statistical methods (median standard deviation) or independent sample-t test and paired sample-t test for comparing data were used. (Data in 95% confidence interval, p value of ≤ 0.05 was considered as statistically significant)
Results
All patients completed surgical intervention without any complication. Surgical procedures were; bipolar release for torticolis, intramedullary pin or plate fixation for clavicula fractures, pin fixation for acromyoclavicular seperation, tension band fixation and/or debridement of open proximal humerus fractures, bankart repair for anterior capsular lesions, closed manipulation for restriction of movement, excision of soft tissue tumours. Same surgical procedures were applied to patients in both groups.
Duration of surgery (minutes) group1; 120.00 ± 15.79, group 2; 114.98 ± 30.69. No significant differencies duration of surgery were noted between the groups. Parasthesia was observed within five minutes. Mean onset block (minutes) group1; 13.4 ± 4.42, group2; 14.1 ± 2.21. Sensory block was matured within 16.3 ± 3.7 minutes, and motor block in 22.6± 5.3 minutes for group 1 and 16.3 ± 3.7 minutes, and motor block in 22.6± 5.3 minutes for group 2. Mean VAS scores of the groups are 3.45 for group 1 and 3.11 for group 2. Movement of the hand and wrist begun on first 24 hours in postoperative period, full movement of neck, arm and forearm arm was observed witin 36 hours of postoperative period. (Table 2)
Table 2
|
Group I ( n = 30 ) |
Group II ( n = 30 ) |
Age, year |
23.22 ± 16.44 |
22.33 ± 14.43 |
Body weight, kg |
67.88 ± 5.60 |
68.11 ± 8.69 |
ASA status |
I |
I |
Duration of surgery, min |
120.00 ± 15.79 |
114.98 ± 30.69 |
Onset block, min |
13.4 ± 4.42 |
14.1 ± 2.21 |
VAS score |
3.45 |
3.11 |
Motor block |
Complete |
Complete |
Sensory block |
Complete |
Complete |
Analgesic requirements |
Six patients |
- |
Supplemental anesthesia |
Three patients % 10 |
Two patients %6.6 |
Overall results |
excellent 24, good 3, moderate 3 |
excellent 28, good 2 |
Table 2: Patient demographics and anesthetic features of two groups.
Group I: Deep servical plexus block using 30 ml 0.5% bupivacaine, Group II: Combined superficial cervical using 10 ml 0.5% bupivacaine and single injection interscalene plexus block using 20 ml 0.5% bupivacaine, ASA: American society of anesthesiologists, VAS: Visual Analoge Scale.
Minor differences were established in heart rate, systolic pressure and diastolic pressure between the groups. The fifth minute hearth rate after induction of anesthesia, was determined as basal value. In the first group, the decreases in heart rate at 30,60,90,120th minutes according to basal value were found statistically significant (p<0.05). In the second group, the decreases in heart rate at 30,60,90,120th minutes according to basal value were found highly significant (p<0.01).
In first group decreases in SBP measurements at 30,60,90,120,150th minutes were found highly significant (p<0.01). In second group 30,60,90,120,150th were found statistically significant (p<0.05). Decreases DBP in group two at 30,60,90th minutes were significant (p<0.05) while the variations at other times were not significant in group one and two.(Table3) The level of PaO2 and PaCO2 were similar in both of groups. PaCO2 levels increase minimal intraoperatively in deep cervical plexus block and these changes were not statistically significantly different when the two groups were compared.
Pain score assessment of blocks for groups was 3.45-3.11 respectively. We evaluated patients acceptance for technique. There were no complaints about double injection technique noted for group 2 and patients accepted satisfactorily the techniques in two groups. The deep cervical plexus block was performed as excellent in 24 and good in 3 patients, moderate in 3 patients in group 1. The combined block was evaluated as excellent in 28 and good 2 patients in group 2. (Table 2) Only 5 patients required intraoperatively supplemental anesthetic at the site of surgery. They were three patients whom underwent surgery for proximal humeral fracture of group 1 and two patients whom underwent release for torticolis of group 2. Six patients (three of them received supplemental anesthesia) were required analgesic drug in group 1 intraoperatively. Pain medication was performed with 3 miligram midazolam and 50 microgram fentanyle citrate intravenously in this group. No differences could be observed about the requirement of postoperative supplemental analgesia
Table 3
SBP: Sistolic blood pressure.
DBP: Diastolic blood pressureTable 3: Changes of heart rate, systolic blood pressure, diastolic blood pressure according to the groups.
Discussion
Deep cervical block is commonly used for vascular surgical procedures not widely used in orthopaedics.4,9
In our opinion, blockage of cervical plexus provides safe orthopaedic surgery around neck, upper shoulder and clavicular region. Operations such as torticollis procedure and osteosynthesis of clavicular fractures were performed effectively with cervical plexus block. In addition sensory innervation of lower part of cervical plexus provided by supraclavicular nerve and this area (also represents of C4 dermatome) reaches just distal to acromioclavicular joint and even surgery of the upper part of the shoulder is available with cervical plexus block.10 But some transient side effects may occur by deep cervical plexus block. Emergy et al showed PaCO2 levels increased under cervical plexus block and it is mostly related with phrenic nerve blockade (diaphragmatic paresis) invariably occurs with a deep cervical plexus block. 11 Respiratory problems caused by phrenic nerve paresis can be prevented by blocking just superficial part of the cervical plexus. In our series there was no significant PaO2 and PaCO2 changes found in both regional block. In our study, patients were young and general health conditions were good, therefore complications seemed less likely to occur. Another topic is the need of supplemental anesthesia of DCP and SCP is % 53.4 Contrary to this study, in our series the need of supplemental anesthesia was %10 for group 1 and % 6.6 for group two. Stoneham et al did not find any statistically significant differences about supplemental analgesic requirements between deep and superficial cervical blocks.12
Interscalene block provides complete anesthesia for 4-6 hours with minimal intravenous sedation and great patient comfort. Sinardi et al reported interscalene brachial block is an alternative procedure to general anesthesia for shoulder surgery, and consents the anaesthetist to easily control postoperative pain.13 Laurila et al reported after arthroscopic shoulder surgery subacromial bursa block has a minor effect only on postoperative analgesia, whereas an interscalene block with low-dose ropivacaine effectively relieves early postoperative pain and reduces the need for opioids.5
We concluded that compared with classic deep cervical block, combined a single injection superficial cervical plexus block and single injection interscalene block has better effective and practical technique and provide more distal level (arm and elbow) anesthesia when compared to deep cervical block. Interscalene block was less painful than classical cervical plexus block. We found that DCP requires slightly increased anesthesia demands during procedure but combination of SCP with IBP may decrease the anaesthetic and analgesic requirements. Combined block is a safe, in our opinion a preferred technique for providing anesthesia for neck and/or shoulder surgery and even wide surgical procedures for upper extremity surgery. Our investigation showed that sensory and motor anesthesia levels, findings of hemodynamic as SBP/DBP, and PaO2 and PaCO2 levels were similar of both technics. But some patient require sedative and analgesic drug in both groups. Patients received high acceptance and we thought that deep cervical plexus block is suitable for neck and clavicular orthopaedic procedures and may be considered as a useful alternative to general anesthesia. Additional local anesthesia should be required in the course of distal shoulder surgery.
References
- Conn RA, Cofield RH, Byer DE, Linstromberrg JW. Interscalene block anesthesia for shoulder surgery. Clin Orthop 1987; 216:94-98.
- Kuflik P, Ankolekar A, StuchinSA, Steinbach S, Bernstein R. Interscalene brachial plexus block anesthesia for upper extremity surgery. J Hand Surg 1986;11-A (2):246-248.
- Pollock RG, Duralde XA, Flatow EL, Bigliani LU. The use of arthroscopy in the treatment of resistant frozen shoulder. Clin Orthop 1994;304:30-36.
- Davies MJ, Silbert BS, Scott DA. Superficial and deep cervical plexus block for carotid artery surgery: a prospective study of 1000 blocks. Eur J Vasc Endovasc Surg 1997;13:37-42.
- Laurila PA, Lopponen A, Kanga-Saarela T. Interscalene brachial plexus block is superior to subacromial bursa block after arthroscopic shoulder surgery. Acta Anaesthesiol Scand 2002;46(8):1031-6.
- Putz R, Pabst R, editors. Sobotta atlas of human anatomy. München- Jena, Urban & Fisher; 2001.
- Canale ST, Beaty JH, editors. Champbell,s operative orthopaedics. Eleventh edition Philedelphia, Pennsylvania: Mosby- Elsevier; 2008
- Moore DC editor. Regional Block, 4th Edn. Springfield, Illinois: Charles C. Thomas, 1979.
- Merle JC, Mazoit JX, Dessgranges P. A Comparison of two techniques for cervical plexus blokade: evaluation of efficacy and systemic toxicity. Anesth Analg 1999;89(6):1366-70.
10. Masters RD, Castresana EJ, Castresana MR. Superficial and deep cervical plexus block: technical considerations. AANA J 1995;63(3):235-43.
11. Emery G, Handley G, Davies MJ. Incidence of phrenic nerve block and hypercapnia in patients undergoing carotid endarterectomy under cervical plexus block. Anaesth Intensive Care 1998;26(4):377-81.
12. Stoneham MD, Doyle AR, Knighton JD, Dorje P. Prospective, randomised comparison of deep or superficial cervical plexus block for carotid endarterectomy surgery. Anaesthesiology 1998;89(4):907.
13.Sinardi D, Chillemi S, Marino A. 0.25% levo-bupivacaine for interscalene block during shoulder surgery. Minerva Anestesiol 2002;68(7-8):589-92.
|