|
Abstract Background:
The treatment of the distal intraarticular radius fracture is
controverse discussed. Dorsal displaced,
unstable and intraarticular compression fractures of the distal
radius are commonly treated by external fixations, K wires or
open reduction and internal fixation (ORIF) with dorsal plating.
If instability criteria are encountered with bone grafting. All
afore mentioned methods show significant morbidity and do not
provide stability. Functional loss after immobilisation,
secondary loss of reduction, pininfections, tendon ruptures and
M.Sudeck are commonly encountered complications. These
results after common distal radius fracture treatment and with
special regard to interference with the surrounding soft tissue,
have encouraged us to stabilize dorsal displaced unstable and
intraarticular fractures through a palmar approach.
Methods: We describe the surgical treatment with
approach, technique of new minimal invasive reduction an
internal ankle stable fixation, our results obtained with this
method over 1 year with 81 patients (AO
classification A: 24.7%, B: 6.2%, C: 69.1%). Using this palmar
approach and the minimal invasive open reduction technique, new
internal fixation device utilizing the locking compression plate
with fixed angle screws, we avoid the soft tissue problems
associated with dorsal plating. We achieve also by
intraarticular fractures stability for functional treatment and
last but not least, we don’t need bone grafting.
Results: A follow up time of 12
months the fractures heated with highly satisfactory
radiographic, and functional results, mean age 54,3 years. The
overall outcome according to the Gartland and Werley score
showed 49% excellent, 41% god, 9%fair and 1% poore results. DASH
Score 15 points after 12 months (before trauma 6,8). Our
experience indicates that all types of distal dorsal displaced
and intraarticulare radius fractures can be anatomically reduced
and fixed through a palmar approach without loss of reduction
results.
Conclusions: This technique offers in our opinion
several advantages: the stronger palmar cortex of the radius, no
tuch from the vascularisation of the bone, possibility of
minimal invasive reduction. The combination
of minimal invasive reduction and stable internal fixation with
preservation of the dorsal soft tissues rapid functional
treatment resulted in rapid healing, no need for bone grafting
no incidence of tendon problems in our study in young such as
older patients
J.Orthopaedics 2006;3(3)e12
Introduction:
Distal radius fractures account for 17% of all fractures, the
incidence is 2/1000/year making this fracture the most commonly
seen traumatic fracture. The treatment is complicated by the
broad range of encountered fracture types and the association
with intraarticular ligamentary injuries. Especially dorsal
open reduction and internal fixation (ORIF) techniques show
numerous anatomical and implant–related problems. The incidence
of extensor tendon complications including irritations
tendonitis, attrition and ruptures secondary to direct contact
of these structures with dorsal plates is not negligible (3,13).
A complication rate greater than 15% is reported for external
fixators leading to unsatisfying results (9). Dorsal ¼ tube
plates usually necessitate spongy bone grafts and prolonged cast
immobilization as well as a longer hospital stay. K wires are
not applicable to complex fractures and extend the range of
complications with PIN infections or symphatic reflex dystrophy.
Hahnloser et al (7) reports more than 15% complications in a
study with Pi plates. Taking into account these commplications
using common implants and a dorsal approach we opted for a
palmar operation technique and the application of angle stable
LCP-plates (10,12). This technique offers in our opinion several
advantages: the stronger palmar cortex of the radial epiphysis
with the additional anatomical advantage of non adherent
neurovascular and tendinous structures. The major advantage
seems to be the far superior soft tissue implant coverage
through the pronator quadratus muscle as well as the overlying
flexor tendons. The locking compression plate is very
suitablefor the palmar approach due to its ability to securely
stabilize dorsal displaced fractures with head locking screw,
precluding any angutytory instability (11).
This new concept “do it the other way”
necessitates a reevaluation of traditional treatment concept of
distal extension and intraarticular displaced fractures of the
radius (12). As there are only few preliminary studies without
long prospective follow up. We have designed a prospective study
to evaluate the clinical outcome of palmar stabilized distal
fractures with angle stable LC Plates. We describe the surgical
treatment with approach, technique of new minimal invasive
reduction and internal fixation, our results obtained with this
method.
Method and materials
From August 2001 – June 2004 (mean follow up 12 months) we
included 81 patients in our prospective study. The distal radius
fractures were classified according to AO (13). There were A
(24,7%), B (6,2%), C (69,1%) fracture types. 34 men, 57 woman
with an mean age 54,3 + 3,7 years (range 18 – 89 years). To
evaluate the effectiveness of palmar fixed angle stable locking
compression plate of distal radius fracturesinformed consent was
obtained from all patients. Criteria for study inclusion were
one or more instability signs. After an initial attempt of
closed reduction radiographic evidence of a persisting deformity
of >15° of angulation in any plane, >2mm of articular
displacement, or >3mm radial shortening defined the fracture
type as unstable. Open fractures were excluded.
The causes of injury were mostly falls on the outstretched
hand (73%), work related accidents (4%) , car accidents (1%) or
sport injuries (12%). Before treatment 4 patients had developed
median nerve symptoms. Mostly all had developed severe soft
tissue swelling and pain with limitation of finger mobility that
persisted for 3 days despite anti inflammatory medication and
elevation of the forearm.
Preoperative radiographic evaluation showed an average dorsal
angulation of -21,4° average radial inclination of 11,8°,
average incongruity (step off , gap) 3,5mm. The time interval
between injury and operation averaged 1 – 10 days, 86% had
regional plexus, 14% general anesthesy. Follow up exams
comprised clinical and radiological evalutation and scoring
after 2,4,6 weeks, 6 and 12 months, according Gartland/Werley
(4) and DASH Score (5). Result and functional outcome was
measured by wrist, finger and forearm motion with goniometer,
Jamar dynamometer and compared with the contralateral side.
Surgical strategy
Palmar approach:
If patients could not be operated on day 1, closed reduction
under local anesthesia and cast immoblisation was performed
initially. Definitive surgical stabilization until day 10 was
achieved in all cases. The operation was performed mostly under
axillary plexus anesthesia with an arm tourniquet inflated to
250- 280mmHg. We chose a radiopalmar approach without routine
incision of the flexor retinaculum for decompression of median
nerve. The skin incision was centered over the Flexor carpi
radialis (FCR) tendon with a length of 5 to 6 cm including the
option of entering the carpal tunnel. A longitudinal incision of
the palmar and dorsal FCR tendon sheats which form the lower arm
fascia, was performed. Radially oriented we
carried out a blunt dissection between the fascia of the flexor
digitorum muscles (FDS and FDP) and the flexor pollicis longus
muscle (FPL).

Here its very important to coagulate two nutrition vessels
of the FPL tendon to avoid arterial bleeding after release of
the tourniquet. Reaching the parona space under the flexor
tendons, FCR, the median nerve and the remaining tendons are all
hold ulnary. After exposing the pronator quadratus muscle we
incised it radially to retract it to the ulnar side. Frequently
seen destruction or interposition of the distal muscle region in
between the fracture fragments neccessitate partial resection.
Direct visualization of the fracture is now easily achieved,
without arthrotomy, preserving the palmar capsular structures.
This allows additional ligamentotaxis for fracture reduction, a
condition for minimally traumatic reduction.
Minimally traumatic reduction technique :

Our intention was to develop a minimally traumatic reduction
technique without extended approach to the joint surface and
without forced gross maneuver (Fig 1), to avoid soft tissue
damage apart from the fracture elements with more consecutive
destruction and danger of reflex dystrophy. The key point is the
ligamentotaxis for this technique (12). Anatomical reduction is
achieved by palmar introduction of 1.4mm K wires into the
fracture gap, which are then used as levers to reduce the palmar
dislocation. Performing gentle lever
maneuvers the anatomical position of even severly displaced
fragments can be reestablished easily and quickly.
Ligamentotaxis assures correct reduction (6).
So you achieve restoration of the anatomic
continuity of the palmar cortex, restore the radial length,
ulnar inclination and mostly the articular congruency of the
joint surface. If not, one can repeat the same technique using a
1.4 or 1.7 mm K wire to raise the joint with subtle lever
movements from within the fracture gap.
To achieve palmar tilt an additional dorsal reduction is
frequently necessary. It’s obtained by dorsal percutaneous
intrafocal insertion of K wires, moving them in distal direction
until the right position is reached. A dorsal 3.5 mm oblique
Titanium LC Plate is then applied palmarly, 3 cancellous screws
are inserted into the proximal plate holes. Direct digital
pressure and counter pressure as well as K wire manipulation of
the distal fragments optimize the fracture reduction prior to
devinite retention with 2-3 head locking screws in the distal
oblique T part of the plate. Placement of the subchondral
support pegs 2-3 mm below the subchondral bone is essential or
optimal fixation, especially in cases with osteoporotic bone
(Fig 2). By this procedure the angular stabilization of the
fracture is secured. Optional dorsal bone grafting through a
small dorsal incision is still possible, but was not performed
in our study group. All K wires are then removed. In isolated
cases involving C 3 fractures one or two K wires for joint
surface reduction were applied percutaneously. The above
described technique obviates any gross reduction maneuvers.
Operations were followed by cast immobilization for 0-4 weeks
according to fracture type and bone stock quality.
Statistical Analysis
Statistical analysis was performed using SPSS 10.0.
Results are expressed as mean ± SEM. Comparisons between
multiple groups were assessed by one-way analysis of variance,
including a modified least-significant difference (Bonferroni)
multiple range test to detect significant differences
between two distinct groups, which were further analyzed using
the Mann-Whitney U test. The strength of the relationship
between two variables was assessed by calculation of the
product-moment correlation coefficient (r). Statistical
significance was accepted at the level of p < 0.05.
Results
In all cases we saw a timely ( 6 weeks) fracture
consolidation, no non- or malunions were encountered. The
intraoperatively attained fracture reduction was good. The mean
follow up time was 10,6 months. AO classification included: A
(A2: 6,2%, A318,5%), B (B1: 1,2%, B2: 1,2%, B3: 3,7%), C (C1:
14,8%, C2: 27,1%, C3: 27,2%). All fractures healed with highly
satisfactory radiographic and functional results: Palmar tilt
angle pre operatively –21,4°, 1- 3 days postoperatively 5,7°.
Pre operatively radial shift 11,7°, 1-3 days postoperative
dorsal shift 24,8°, pre-operative ulnar variance 3,5, 1-3 days
post-operative ulnar variance 0 mm. There were no significant
differences in palmar tilt angle, dorsal shift and ulnar
variance between the immediate post-operative In the follow-up
course we saw one patient with loss of reduction in a severly
comminuted C3 fracture and infection. No implant failure was
seen. The overall outcome according to the Gartland and Werley
score showed 41,2% excellent,47,1% good, 9,8%fair and 1,2% poore
results. DASH Score was 15,5 points after 12 (before trauma
6,8). Mobility of the wrist is shown in the Tab 1. The following
complications were observed (Fig 3) : infection 1, crps 1,
rupture of FPL tendon 1 (wrong operation technique, see Fig 3).
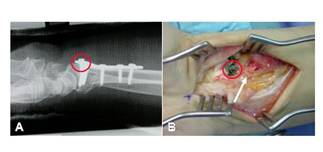
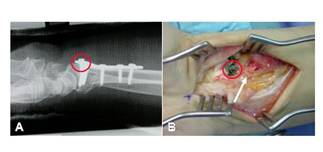
Figure 3: A: Dislocated screw after insuffizient
technique surgery (cicle). B: This follows in a Flexor pollicis
longus ruptur (arrow)
Discussion :
The need for dorsal dissection from extensor sheats,
periosteum, retinaculum, and vascular supply to dorsal
metaphyseal fragments, need of bone graftingand different
complications such as tendonitis, rupture of tendons, reflex
dystrophy, immobilization damage or technique damage (long time
fixateur externe)(1), secondary displacement due to loosening of
the distal screws (seen in Pi Platesand osteoporotic bone)(2)
encouraged us to develop an new concept treatment “do it the
other way”. With the locked compressed angle stable Titan plate,
we have an implant to perform a stabil internal fixation that
would prevent fracture collaps. With the palmar approach we have
an easy and fast access to the fracture. With our minimally
traumatic reduction technique using manually guided K wires and
ligamentotaxis we avoid gross interference with the surrounding
soft tissue. Covering the plate completely
the pronator quadratus muscle prevents the overlying tendons
from any damage. So we had no complications with tendon
irritations or reflex dystrophy. Compared with other functional
treatments we had the same outcome of functional results (8).
Tab 1 : Functional wrist mobility 12
month after operation of distal radius fracture
|
Wrist mobility
(Neutral/Zero
method, °) |
Normal range
(mean) |
After 6 months
mean (+ x) |
After 12 months
mean (+ x) |
|
Flexion/Extension
Ulnar/Radialduction
Pro-/Supination |
60 – 0 – 60
40 – 0 – 30
90 – 0 – 90 |
48(+13,9) – 0 -
54(+13,9)
30(+9,4) – 0 -
19(+7,7)
78(+16,3) – 0 -
75(+18,3) |
53(+14,3) – 0 -
61(+16,4)
33(+8,4) – 0 -
22(+6,4)
81(+17,2) – 0 -
78(+17,2) |
In our experience we saw, that’s very easy to reduce A or B
type fractures and perform the internal fixation. If the bone is
osteoporotic or it’s an intraarticular C type fracture you have
to consider the following hints to achieve a save and stable
reduction result:
1.The distal pegs must be introduced as closely as possible
to the subchondral plat of joint to prevent loss of reduction
especially in osteoporotic bone or as a result of early
functional treatment.
2.Before applying the plate, it’s important in intraarticular
fractures to reach a good articular congruency of the joint
surface (K wire through the fracture combined with
ligamentotaxis = minimally traumatic technique), and a good
reduction of the palmar cortex. This maneuvre restore good ulnar
inclination and axial, radial length. Then you apply the T Plate
with proximal screws. On the plate, with K wirs from dorsal or
distal stable screws exactly behind the subchondral plate you
can raise the palmar tilt in the right position. After that you
fix the distal angle stable screws definitively.
3.For early functional treatment of intraarticular fractures
it’s important that you fix the outer ulnar and radial
fragments. Without this you must be aware of a secondary
fracture displacement especially in the distal radio-ulnar
joint.
Conclusion
Our results show that open reduction and palmar internal
fixation with an angle stable dorsal T plate in combination with
a minimally traumatic reduction maneuvre is an exellent
possibility for the treatment of distal radius fracture,
especially in dorsally displaced or intraarticular fractures.
In our learning curve we saw by intraarticular fractures you
must consider the experience below: correct subchondral position
of the screws, seize the radial an ulnar fragments.
Our experience shows that because of the
ligamentotaxis the use of minimally traumatic reduction
maneuvers lead to best results in articular congruency and
fracture reduction. "Don’t touch to
much!"
Reference :
- Basten K, Hansen M, Rommens PM. Die
operative Behandlung der distalen Radiusfraktur durch
T-Plattenosteosynthese. Akt Traumatol 29:137-143. 1999.
- Carter PR, Frederick HA, Saseter GF.
Open reduction and internal fixation of unstable distal radius
fractures with a low profile plate: a multicenter study of 73
fractures. J Hand Surg Am 23:300-307. 1998.
- Fernandez DL. Should anatomic reduction
be pursued in distal radial fractures? J Hand Surg
2000.25B1-6.
- Gartland JJ, Werley CW. Evaluation of healed Colles –
Fractures. J Bone Joint Surg Am 33: 895-907. 1951.
- German G, Wind G, Harth A. Der DASH-Fragebogen.
Ein neues Instrument zur Beurteilung
von Behandlungsergebnissen an der oberen Extremität. Handchir
Mikrochir Plast Chir 31:149-150. 1999.
- Greatting MD, Bishop AT. Intrafocal (Kapandji)
pinning of unstable fractures of the distal radius. Orthop
Clin North Am 1993:24:301-307.
- Hahnloser D, Platz A, Amgwerd M, Trentz O. Internal
fixation of distal radius fractures with dorsal dislocation:
Pi Plate or two ¼ tube plates? A prospective randomized study.
The Journal fo Trauma 47: 760-765. 1999.
- Jakob M, Rikli DA, Regazzoni P.
Fractures of the distal radius treated by internal fixation
and early function: a prospective study of 73 consecutive
patients. J Bone Surg. 82B:340-344. 2000.
- Jupiter JB, Fernandez MD, Choon-Lai Toh et al. Operative
treatment of volar intraarticular fractures of the distal end
of the radius. J Bone Joint Surg Am 78:1817-1828. 1996.
- Letsch R, Infanger M, Schmidt J, Kock H. Surgical
treatment of fractures of the distal radius with plates: a
comparison of palmar and dorsal plate position. Arch Orthop
Trauma Surg 123: 333.339. 2003.
- Orbay J, Fernandez D. Volar fixation
for distally displaced fractures of the distal radius: A
preliminary report. J of Hand Surg. 27:2. 2002.
- Stahel P, Infanger M, Bleif M, Heyde
C, Ertel W. Die palmare winkelstabile Plattenosteosynthese.
Ein neues Konzept zur Versorgung instabiler distaler
Radiusfrakturen. Trauma und Berufskrankheiten. 2004.
- Zettl RP, Rucholtz S, Taeger G, Obertacke
U, Nast-Kolb D. Postoperative Morbidität der operativ
behandelten distalen Radiusextensionsfrakturen. Unfallchirurg
104 : 710-715.2001.
|