|
*Sanket Diwanji # Gautam Zaveri
*Consultant Orthopaedic Surgeon, Akshar Purshottam Arogya
Mandir & Muni Seva Ashram ,Goraj, Vadodara, India
#Consultant Orthopaedic Surgeon, Akshar Purshottam Arogya Mandir &
Muni Seva Ashram ,Goraj, Vadodara, India
Address for Correspondence
Dr. Sanket R Diwanji,
B-201, Jaltarang Apartment,Halar Cross Road, Valsad,
GUJARAT, INDIA, 396001
Phone:919825658983
FAX:(02668)268048
E-MAIL: sanket_diwanji@yahoo.co.in |
|
Abstract
Spinal tuberculosis is often associated with
a pre or paravertebral abscess. In most instances, an abscess in
the psoas muscle can be drained by CT/ Ultrasound guided
aspiration, by endoscopy or by an open surgery during anterior
debridement of the vertebrae.
In two patients with dorsal spine tuberculosis where a posterior
midline incision had been used for debridement, decompression
and stabilization, we have extended the incision caudally and
used an intertransverse approach to drain the associated psoas
abscess. A thorough evacuation of the abscess was possible and
both patients went on to heal uneventfully.
The intertransverse approach has been routinely used for the
excision of a foraminal disc herniation but its use has not been
reported for the drainage of a psoas abscess. Operative
technique, clinical feasibility and postoperative results are
discussed.
Keywords: Inter transverse approach, psoas abscess
J.Orthopaedics 2006;3(1)e10
Introduction:
A psoas abscess is a common sequelae to
tuberculosis of the dorsolumbar spine. Various methods of
drainage of psoas abscess have been described. Open drainage can
be done posteriorly through the Petit`s triangle, laterally by a
flank incision parallel to the crest of the ilium, anteriorly
under the Poupart ligament or by a Ludloff incision when the
psoas abscess points subcutaneously in the adductor region of
the thigh1. Ultrasound or CT guided percutaneous drainage and
retroperitoneoscopic drainage is also described2,3,4,5.
We report two patients with tuberculosis of
the dorsal spine who underwent a transpedicular decompression
and instrumented stabilization. The concomitant psoas abscess
was drained using an intertransverse approach after extending
the posterior incision caudally. The intertransverse approach as
described by Wiltse has gained popularity for removal of far
lateral disc herniation6,7, but its application for drainage of
psoas abscess has not been described.
Case Report:
Surgical Technique:
Case 1:
A thirty-two year old female presented with
severe persistent lower dorsal back pain without neurological
deficit. She had been treated with antituberculous drugs for
eight months before coming to us, but continued to worsen. As
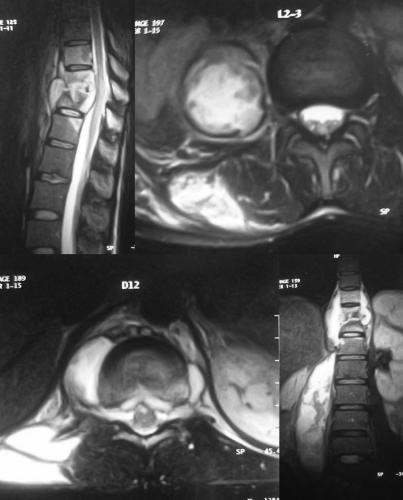
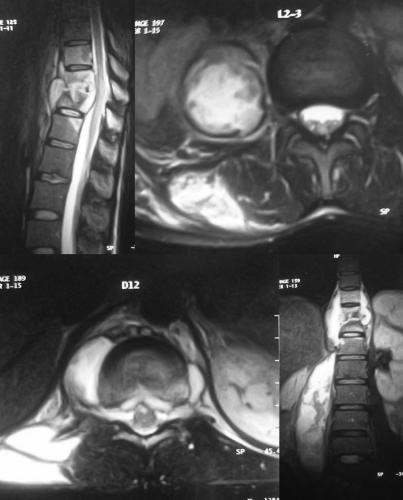
shown in Fig.1, the MRI scan revealed destruction at D11/12
vertebrae with a prevertebral abscess, abscess in epidural
space, unilateral psoas abscess and a posterior paraspinal
abscess.
She was operated using a posterior midline
incision. Bilatertal costotransversectomies were done at D11
level to drain the paravertebral abscess. The anterior lesion
was then debrided through a transpedicular approach and
cancellous graft from the laminae and spinous process was packed
in the anterior defect. Posterior stabilization was done using a
rod-screw construct from D10 to L1 vertebra. The posterior
paraspinal abscess was drained. The incision was then extended
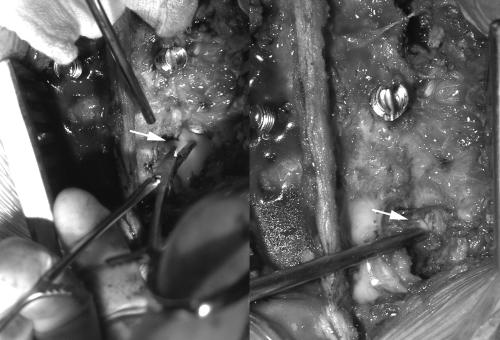
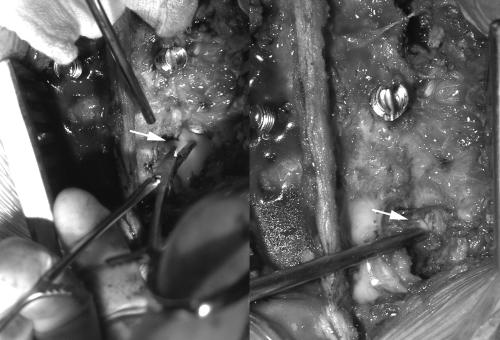
caudally up to the L3 vertebrae. As shown in Fig2 the
intertransverse membrane was elevated between the L 2 & L3
transverse processes on the affected side. The psoas muscle
appeared bulky. Pus was aspirated with a 16G needle to confirm
location. The muscle was then incised and the abscess cavity was
thoroughly evacuated. Approximately 400cc of thick pus was
drained and the incision was closed over an intercostal (wide
bore) drain. Postoperative period was uneventful. The drain was
removed on the fifth post-operative day. Antituberculous drugs
were continued for one year. The tuberculosis healed and she
went on to a solid fusion. At twenty months follow-up she
continues to do extremely well.
Case 2:
 A
twenty six year old male presented with pain in the lower dorsal
region for one year, progressive weakness in the lower limbs and
inability to walk with loss of bladder control. Examination
revealed a painful gibbus at D9, grade 1 power in both lower
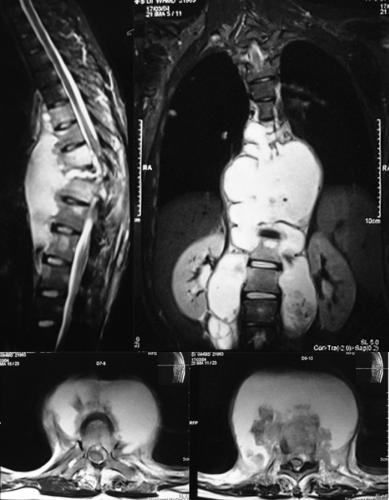
limbs, hypoaesthesia below D10, with bladder involvement. As
shown in Fig 4 his MRI scan showed destruction of D 9 vertebral
body with kyphosis and severe spinal cord compression due to
epidural granulation/ abscess. There was a prevertebral abscess
extending A
twenty six year old male presented with pain in the lower dorsal
region for one year, progressive weakness in the lower limbs and
inability to walk with loss of bladder control. Examination
revealed a painful gibbus at D9, grade 1 power in both lower
limbs, hypoaesthesia below D10, with bladder involvement. As
shown in Fig 4 his MRI scan showed destruction of D 9 vertebral
body with kyphosis and severe spinal cord compression due to
epidural granulation/ abscess. There was a prevertebral abscess
extending
 from
D 6 to D12 resulting in scalloping of the anterior surface of
the vertebral bodies as well as bilateral psoas abscesses. The
vertebral bodies were quite osteoporotic due to long standing
disease. He had been treated with alternative medicines for 8 to
9 months and antituberculous drugs for 3 months before
presenting to us with the above picture. from
D 6 to D12 resulting in scalloping of the anterior surface of
the vertebral bodies as well as bilateral psoas abscesses. The
vertebral bodies were quite osteoporotic due to long standing
disease. He had been treated with alternative medicines for 8 to
9 months and antituberculous drugs for 3 months before
presenting to us with the above picture.
 He
was operated through a posterior midline incision. Pedicle
screws were inserted in D7, D8, D10 & D11 vertebrae. Bilateral
costotranversectomy enabled us to drain the prevertabral
abscess. Through a transpedicular approach, the remnants of the
D9 body with the D8/9 and D9/10 disc were excised and the spinal
cord was decompressed. Cancellous chip graft obtained from the
lamina was then loosely packed in the intervertebral area. Rods
were assembled and compression was done in order to achieve a He
was operated through a posterior midline incision. Pedicle
screws were inserted in D7, D8, D10 & D11 vertebrae. Bilateral
costotranversectomy enabled us to drain the prevertabral
abscess. Through a transpedicular approach, the remnants of the
D9 body with the D8/9 and D9/10 disc were excised and the spinal
cord was decompressed. Cancellous chip graft obtained from the
lamina was then loosely packed in the intervertebral area. Rods
were assembled and compression was done in order to achieve a
 vertebral
shortening (pedicle substraction) effect. Posterior
decortication and bone grafting was done at the instrumented
levels. The incision was extended into the lumbar spine. The
intertransverse membrane was elevated bilaterally at L1/2 level
and the approximately 250 cc pus was drained from the psoas
abscess both on the right and the left. The wound was closed
over a wide bore drain placed in both the psoas muscles. Drains
were removed on the fifth post-operative day. The postoperative
period was uneventful. Antituberculous drugs were continued. At
10 months follow-up, the patient is pain free, has fully
recovered neurologically. Xrays showed early consolidation
between D8 and D10. vertebral
shortening (pedicle substraction) effect. Posterior
decortication and bone grafting was done at the instrumented
levels. The incision was extended into the lumbar spine. The
intertransverse membrane was elevated bilaterally at L1/2 level
and the approximately 250 cc pus was drained from the psoas
abscess both on the right and the left. The wound was closed
over a wide bore drain placed in both the psoas muscles. Drains
were removed on the fifth post-operative day. The postoperative
period was uneventful. Antituberculous drugs were continued. At
10 months follow-up, the patient is pain free, has fully
recovered neurologically. Xrays showed early consolidation
between D8 and D10.
Discussion :
Spinal tuberculosis typically results in
destruction of vertebrae and formation of soft-tissue abscesses
that may eventually result in kyphotic deformity and
neurological deficits. Surgery is aimed at debridement of the
devitalized vertebrae, decompression of spinal cord/ nerve roots
and spinal fusion. Anterior or posterior instrumentation is used
to reduce the incidence of graft related complications as well
as maintain sagittal alignment. A paravertebral abscess in the
thoracic spine or a psoas abscess is often drained to reduce the
bulk of diseased tissue and promote healing. Whilst anterior
instrumentation to supplement anterior fusion is an accepted
procedure, anterior instrumentation may not be adequate in
patients with severe osteoporosis (due to long standing
disease), or where there is involvement of multiple vertebrae.
Occasionally anterior surgery may be contraindicated because of
medical or anaesthetic reasons. In these patients either an
anterior debridement/ decompression & fusion may be followed by
a posterior instrumentation 8,9 or a posterolateral (transpedicular)
debridement and decompression may be supplemented by a posterior
instrumentation 10.
A psoas abscess associated with dorsal spine
disease may not be adequately drained through the transthoracic
approach used for decompression since the pus is very thick and
there may be septa and loculations 11. It may require to be
drained separately either endoscopically or through a separate
incision in the Petit`s triangle posteriorly, along the crest of
the ilium laterally or under the Poupart ligament anteriorly.
This requires a second incision and increases the duration of
surgery and overall morbidity. Such large abscesses usually
cannot be drained adequately by percutaneous technique.
Wiltse & Spencer described the paraspinal
approach to the lumbar spine which involves longitudinal
separation of the sacrospinalis muscle group to expose the
posterolateral aspect of lumbar spine12. The intertransverse
membrane is then elevated from its attachment to the transverse
processes to visualize the exiting nerve root and excise a far
lateral disc herniation. As illustrated in Fig6, anatomically
the psoas muscle takes origin from the anterior surface of the
transverse processes of the lumbar vertebral bodies. Thus once
the intertransverse membrane is elevated, the muscle seen
immediately anteriorly is the psoas muscle. An incision made on
the posterior surface of the muscle enables us to access the
abscess cavity and thoroughly drain the abscess leaving behind a
wide bore drain for further drainage post-operatively. In Case
no1, the patient had D11/12 tuberculosis with prevertebral,
epidural, right posterior paraspinal abscess/ granulation with a
huge abscess in the right psoas muscle. Using the traditional
anterior approach, she would have required a right sided
anterior transdiaphragmatic approach for debridement,
decompression and drainage of the psoas abscess followed by a
drainage of the posterior paraspinal abscess. Besides the long
standing disease had resulted in significant osteoporosis of the
vertebrae, so that the likelihood of problems with anterior
instrumentation was higher. Through the posterior approach, we
were able to drain the paraspinal abscess, the prevertebral
abscess, perform a transpedicular debridement, decompression and
instrumented fusion. Finally by elevating the intertransverse
membrane in the lumbar spine, we identified the psoas muscle and
under vision drained it completely thereby fulfilling all the
aims of the surgery through a single, cosmetic incision whilst
reducing the morbidity associated with a combined anterior &
posterior procedure.
In case 2, the patient had destruction of D9
with spinal cord compression. His vertebral bodies were again
very osteoporotic and the anterior surfaces of the bodies from
D6 to D12 were scalloped because of the pressure from the
longstanding anterior paravertebral abscess. Anterior
instrumentation alone in these circumstances would have a high
risk of failure. Besides separate incisions would be required to
drain the large bilateral psoas abscesses. Here again we elected
to perform the entire procedure posteriorly. We instrumented
from D7 to D11, drained the prevertebral abscess by bilateral
costotransversectomy at D9, then resected the D9 vertebra
through a transpedicular approach and finally compressed between
the cephalad and caudad screws to achieve vertebral shortening.
The last step was to extend the midline incision downwards and
through a bilateral intertransverse approach between L1 and L2,
drain both the psoas abscesses. Again the entire procedure was
safely performed through a single incision.
Thus in both instances, we found that the
intertransverse approach directly led us to the psoas abscess
cavity. We were able to evacuate the cavity thoroughly and leave
a wide bore drain for evacuating subsequent collection. In
patients with a dorsal or lumbar tuberculosis, where posterior
surgery is being contemplated, the intertransverse approach is
an easy, safe and efficient method to drain the associated psoas
abscess through the same posterior skin incision. This reduces
duration and morbidity of surgery. Further bilateral psoas
abscess can be drained through a single incision
Conclusion:
In patients with dorsal or lumbar spine
tuberculosis undergoing a posterior debridement, decompression
and stabilization, the intertransverse approach permits
excellent drainage of the psoas abscess through an extension of
the same posterior midline incision and without any significant
additional morbidity.
Reference :
-
Campbell’s operative orthopaedics.10th
edition, page 2047
-
Dinc H ,Onder C , Turham A U , Suri A,
Aydin A, Yulung G Gumele HR .Percutaneous catheter drainage of
tuberculous and non tuberculous psoas abscess. Eur. J.
Radiology.1996 Sep ; 23(2):130- 4
-
Gupta S, Suri S, Gulati M, Singh P .Ilio-psoas
abscess :percutaneous drainage under image guidance. Clin
Radiology 1997 Sep;52(9):704-7
-
Katara AN, Shah RS, Bhandarkar DS, Unadkat
RJ. Retroperitoneoscopic drainage of a psoas abscess. J.
Paediatr.Surg.2004 Sep;39(9)C 4-5
-
Kang M , Gupta S, Gulati M, Suri S .Iliopsoas
abscess in the paediatric
-
Population: treatment by US –guided
percutaneous drainage. Paediatr Radiol.1998 Jun; 28(6):
478-81
-
Greiner-Perth R, Bohm H, Allan Y. A new
technique for the treatment of lumbar far lateral disc
herniation technical note and preliminary result .Eur. Spine
J.2003;12(3):320-4 Epub 2002 Dec 11
-
Hodges S D, Humphray SC, Eck J C,
Covington LA .The surgical treatment of far lateral L 3-4 &
L4-5 disc herniations modified technique & outcome analysis of
25 patients. Spine.1999 Jun 15;24(12):1243-6
-
Mukhtar AM , Farghaly MM, Ahmed SH.
Surgical treatment of thoracic and lumbar tuberculosis by
anterior interbody fusion and posterior instrumentation. Med
Princ Pract .2003 Apr-Jun;12(2):92-6.
-
Benli I T , Akalin S ,Citak Kis M, M,
Kanevetei S , Duman E,. The results of anterior radical
debridement and anterior instrumentation in pott’s disease &
comparison with other surgical techniques. Kobe J Med. Sci.
2000 Apr; 46 (1-2) :39- 68
-
Mehta JS, Bhojraj SY Tuberculosis of
thoracic spine A classification based onthe selection of
surgical strategies. J.Bone Joint Surg Br.2001 Aug;83
(6):859-63
-
Iwaki H, Mori H, Kajita Y, Yoshida T,
Yamayuchi T. Giant psoas abscess with aggressive extension:
report of a case. Hinyokiko Kiyo.1999 Dec;45 (12) :835-7
-
Wiltse LL, Spencer CW; New uses &
refinements of the paraspinal approach of the lumbar spine,
Spine 13:696, 1988
|



 A
twenty six year old male presented with pain in the lower dorsal
region for one year, progressive weakness in the lower limbs and
inability to walk with loss of bladder control. Examination
revealed a painful gibbus at D9, grade 1 power in both lower
limbs, hypoaesthesia below D10, with bladder involvement. As
shown in Fig 4 his MRI scan showed destruction of D 9 vertebral
body with kyphosis and severe spinal cord compression due to
epidural granulation/ abscess. There was a prevertebral abscess
extending
A
twenty six year old male presented with pain in the lower dorsal
region for one year, progressive weakness in the lower limbs and
inability to walk with loss of bladder control. Examination
revealed a painful gibbus at D9, grade 1 power in both lower
limbs, hypoaesthesia below D10, with bladder involvement. As
shown in Fig 4 his MRI scan showed destruction of D 9 vertebral
body with kyphosis and severe spinal cord compression due to
epidural granulation/ abscess. There was a prevertebral abscess
extending
 from
D 6 to D12 resulting in scalloping of the anterior surface of
the vertebral bodies as well as bilateral psoas abscesses. The
vertebral bodies were quite osteoporotic due to long standing
disease. He had been treated with alternative medicines for 8 to
9 months and antituberculous drugs for 3 months before
presenting to us with the above picture.
from
D 6 to D12 resulting in scalloping of the anterior surface of
the vertebral bodies as well as bilateral psoas abscesses. The
vertebral bodies were quite osteoporotic due to long standing
disease. He had been treated with alternative medicines for 8 to
9 months and antituberculous drugs for 3 months before
presenting to us with the above picture. 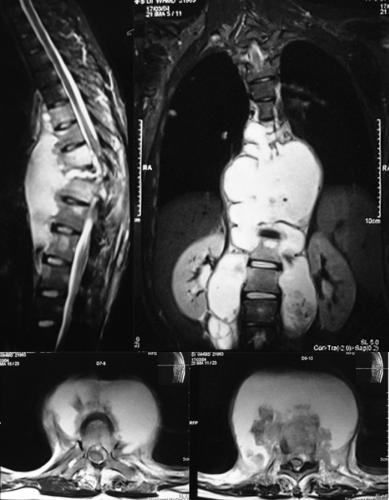 He
was operated through a posterior midline incision. Pedicle
screws were inserted in D7, D8, D10 & D11 vertebrae. Bilateral
costotranversectomy enabled us to drain the prevertabral
abscess. Through a transpedicular approach, the remnants of the
D9 body with the D8/9 and D9/10 disc were excised and the spinal
cord was decompressed. Cancellous chip graft obtained from the
lamina was then loosely packed in the intervertebral area. Rods
were assembled and compression was done in order to achieve a
He
was operated through a posterior midline incision. Pedicle
screws were inserted in D7, D8, D10 & D11 vertebrae. Bilateral
costotranversectomy enabled us to drain the prevertabral
abscess. Through a transpedicular approach, the remnants of the
D9 body with the D8/9 and D9/10 disc were excised and the spinal
cord was decompressed. Cancellous chip graft obtained from the
lamina was then loosely packed in the intervertebral area. Rods
were assembled and compression was done in order to achieve a
 vertebral
shortening (pedicle substraction) effect. Posterior
decortication and bone grafting was done at the instrumented
levels. The incision was extended into the lumbar spine. The
intertransverse membrane was elevated bilaterally at L1/2 level
and the approximately 250 cc pus was drained from the psoas
abscess both on the right and the left. The wound was closed
over a wide bore drain placed in both the psoas muscles. Drains
were removed on the fifth post-operative day. The postoperative
period was uneventful. Antituberculous drugs were continued. At
10 months follow-up, the patient is pain free, has fully
recovered neurologically. Xrays showed early consolidation
between D8 and D10.
vertebral
shortening (pedicle substraction) effect. Posterior
decortication and bone grafting was done at the instrumented
levels. The incision was extended into the lumbar spine. The
intertransverse membrane was elevated bilaterally at L1/2 level
and the approximately 250 cc pus was drained from the psoas
abscess both on the right and the left. The wound was closed
over a wide bore drain placed in both the psoas muscles. Drains
were removed on the fifth post-operative day. The postoperative
period was uneventful. Antituberculous drugs were continued. At
10 months follow-up, the patient is pain free, has fully
recovered neurologically. Xrays showed early consolidation
between D8 and D10.