|
Abstract
Clinical Governance is a
system for improving the standard of clinical practice.It was
first described in a government White Paper as a new system in
NHS Trusts and primary care to ensure that clinical standards
are met, and that processes are in place to ensure continuous
improvement, backed by a new statutory duty for quality in NHS
Trusts.
METHOD: Questionnaires with all the components of
Clinical Governance were distributed amongst 10 doctors, who
included Pre registration House Officers, Senior House Officers
and Registrars, and were requested to complete it by just
ticking the appropriate boxes of Knowledge, Attitude and
Practice regarding a component. These questionnaires were later
collected, analysed and the following results were obtained.
RESULTS: It was indeed a very positive result obtained.
Out of the 10 doctors, all of them were well aware of Clinical
Governance, though not all of them having participated in all
its components. 8 out of 10 doctors, were aware of all the
components of Clinical Governance, and 8 out them had been a
part of majority of the components.
CONCLUSION: It does
emphasise the fact that the NHS is moving towards improvement
and that with growing emphasis on the components of Clinical
Governance, Junior doctors are encouraged to know about it, and
to be a part of it, for the betterment of patient service.
J.Orthopaedics 2006;3(1)e1
Introduction:
Clinical Governance is a
powerful, new and comprehensive mechanism for ensuring that high
standards of clinical care are maintained throughout the NHS and
the quality of service is continuosly improved.
Clinical Governance is a framework through
which NHS organisations are accountable for continuously
improving the quality of their services and safeguarding high
standards of care by creating an environment in which excellence
in clinical care will flourish. Clinical Governance provides the
opportunity to understand and learn to develop the fundamental
components required to facilitate the delivery of quality care
a no blame, questioning, learning culture, excellent leadership,
and an ethos where staff are valued and supported as they form
partnerships with patients. These elements have perhaps
previously been regarded as too intangible to take seriously or
attempt to improve. Clinical Governance demands the re
examination of traditional roles and boundaries between health
professionals, between doctor and patient, and between managers
and clinicians and provides the means to show the public that
the NHS will not tolerate less than best practice.
Literature
Review
Ayers noted there was
uncertainty about clinical governance and how to implement
it.Quality is a major issue in the NHS, but previous initiatives
introduced over the past 20 years, such as resource management,
clinical guidelines and clinical effectiveness, were not
particularly successful in improving the quality of the service
provided.Clinical quality has always engendered a multiplicity
of approaches. Universally accepted definitions have been
difficult to achieve, and some have even considered the term too
subjective to be useful.
The new frame work is
rapidly evolving, with the expectation that quality will improve
incrementally in the future. This framework challenges
clinicians traditional autonomy and will only succeed to the
extent that they find it supportive and helpful.
There are 7 components to
clinical governance, these are:
1. Patient and public
involvement
How we involve patients and carers in their care and clinical
governance activities e.g. research and development. This
includes the patient experience and access to services and
quality of clinical care. An example of measuring this would be
through a patient survey.
2. Clinical risk
management
The system for risk management including the way in which the
different elements, e.g. incidents and complaints are brought
together and how they link with other governance activity.
3. Clinical Audit
This will include how topics are selected and how we report,
implement and follow up recommendations.
4. Clinical
effectiveness
How we implement and apply effective clinical practice e.g.
evidence based guidelines and hence improve the patient
experience and outcomes.
5. Staffing and staff
management
The Trust's approach to human resource management, staff
development and performance, such as appraisals.
6. Education, training
and continuing personal and professional development
The Trust's strategy and plans for education, training and
continuing development, with descriptions of education and
training activities e.g. number of staff who have had mandatory
training.
7. Use of information
to support clinical governance and health care delivery
This involves our strategy and plans for IM&T and how we utilise
information and involve patients to help identify needs.
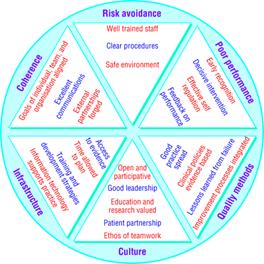
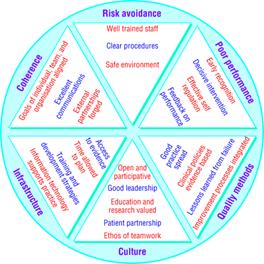
Integrating approaches of
Clinical Governance.
Pie Diagram Showing
the Results obtained.
The questionnaire used and
the results were as follows:
|
Elements: |
Knowledge |
Attitude |
Practice |
|
Clinical Audit |
10 |
10 |
10 |
|
Continual Professional
Development/ Lifelong Learning |
10 |
10 |
10 |
|
Evidence Based
Practice |
10 |
10 |
08 |
|
Clinical Risk
Management and Critical Incidence Reporting |
10 |
10 |
08 |
|
Multidisciplinary Team
working |
10 |
10 |
08 |
|
Research and
Development |
10 |
10 |
08 |
|
Guidelines and
Protocols |
10 |
10 |
09 |
|
Clinical Effectiveness |
10 |
10 |
10 |
Discussion :
Since a variety of variables were used in
this short study, I will refrain myself only to some of them,
which deserve special mention. Herewith I have dealt only with
Clinical Audit, Clinical Effectiveness, and Continuing
Professional Development.
Clinical Audit:
Clinical audit
is a quality improvement process that seeks to improve patient
care and outcomes through systematic review of care against
explicit criteria and the implementation of change. Aspects of
the structure, processes, and outcomes of care are selected and
systematically evaluated against explicit criteria. Where
indicated, changes are implemented at an individual, team, or
service level and further monitoring is used to confirm
improvement in healthcare delivery. This definition is endorsed
by the National Institute for Clinical Excellence.
For clinical
audit to become an important component of how we manage our
health services a very real change needs to take place in the
standing of audit programmes within the NHS. Audit can no longer
be seen as a fringe activity for enthusiasts within
clinical governance, the NHS needs to make a commitment to
support audit as a mainstream activity.
-
Clinical audit
is used to improve aspects of care in a wide variety of
topics. It is also used in association with changes in systems
of care, or to confirm that current practice meets the
expected level of performance.
-
Clinical audit
projects are best conducted within a structured programme,
with effective leadership, participation by all staff, and an
emphasis on team working and support.
-
Organizations
must recognize that clinical audit requires appropriate
funding. Organizations need to recognize that improvements in
care resulting from Clinical audit can increase costs.
-
The
participation of staff in selecting topics enables concerns
about care to be Reported and addressed. Participation in
choice of topic is not always Necessary, but may have a role
in reducing resistance to change.
-
The priorities
of those receiving care can differ quite markedly from those
of Clinicians. Service users should therefore be involved in
the clinical audit Process.
-
There are
practical approaches for user involvement in all stages of
audit, Including the design, the collection of data about
performance, and in Implementing change.
-
Organizations
should ensure that their healthcare staff learn the skills of
Clinical audit.
-
The most
frequently cited barrier to successful clinical audit is the
failure of Organizations to provide sufficient protected time
for healthcare teams.
-
Those involved
in organizing audit programmes must consider various Methods
of engaging the full participation of all health service
staff.
Clinical Effectiveness:
Clinical effectiveness can
be ensured with interventions, which have been shown to be
effective to appropriate patients. It manifests itself in
improved patient outcomes.
The use of clinically effective interventions in practice is
based on:
-
Appraisal of relevant
information or data
-
Dissemination to
relevant staff
-
Adaptation of procedures
to meet local needs
-
Implementation of the
evidence through developing guidelines
-
Evaluation of the change
in practice through clinical audit and analysis of outputs and
outcomes to demonstrate clinical effectiveness in practice.
Although current health
care practice has evolved over the years through personal
experience, expert views and trial and error, there is a great
deal of evidence about clinical effectiveness of services and
treatments. Evidence of cost effectiveness of treatments is
harder to find.
Continuing Professional
Development (CPD):
CPD is the means by which
members of professional associations maintain, improve and
broaden their knowledge and skills and develop the personal
qualities required in their professional lives.
Continuing Professional
Development is a continuous process of personal growth, to
improve the capability and realise the full potential of
professional people at work.
This can be achieved by
obtaining and developing a wide range of knowledge, skills and
experience, which are not normally acquired during initial
training or routine work, and which together develop and
maintain competence to practise.
There are a number of
reasons why one may wish to undertake CPD, including:
|
|
The desire to develop
professional knowledge and skills. |
|
|
A condition placed on
continuing membership of a professional body. |
|
|
To demonstrate
professional standing to clients and employers. |
|
|
To assist with career
development or a possible career change. |
In the NHS, CPD is determined
through appraisal with a personal development plan agreed
between the individual professional and their manager with the
commitment of the necessary time and resources. A key
development in ensuring that health professionals maintain their
competence is the move among the regulatory bodies to develop
CPD strategies for the revalidation/re-certification of their
members.
There are, however, certain
principles that those involved in CPD may want to bear in mind.
-
CPD contributes to improved
patient healthcare and to a healthier society.
-
Each individual is
responsible for taking part in and recording their own
relevant CPD activities.
-
CPD also helps doctors to
improve their professional effectiveness, career opportunities
and work satisfaction.
-
CPD should cover all areas
of Good Medical Practice. Doctors should keep up to date in
all areas of their practice.
-
Doctors should also
recognise when unexpected opportunities for CPD arise and
should allow time to consider and discuss these opportunities
informally. A range of different activities will normally be
suitable.
-
CPD should also include
public and patient involvement. For example, patients and the
public should be involved in developing CPD schemes, setting
standards and monitoring quality. Doctors must be up to date
with what patients and the public expect.
-
Doctors should discuss and
review their CPD with others. Yearly appraisal gives a formal,
structured opportunity for doctors to discuss their CPD needs.
Appraisal provides a way of making sure that any CPD
identified is relevant to a doctor's practice and learning
needs. Doctors should use personal development plans to make
sure that they, their organisations and patients benefit as
much as possible from their CPD.
-
Assessment measures, where
available, should be used for part of doctors' CPD. These
measures should allow doctors to be clear about how they are
developing. They will help doctors to judge their progress.
Valid and reliable assessment tools and systems are still
developing. (Indeed, developing these tools would be a
valuable CPD activity for doctors.)
Individual doctors need to
keep themselves up to date in all areas.
These are:
ุ good professional
practice;
ุ maintaining good
medical practice;
ุ relationships with
patients;
ุ working with
colleagues;
ุ teaching and training;
ุ probity; and
ุ health.
Acknowledgement:
I wish to thank Mr. Nicholas
Garlick, Consultant Orthopaedic Surgeon, for his invaluable help
and suggestions,
without which this venture would have been impossible. My
sincere thanks to the Department of Orthopaedics at the Royal
Free Hospital, London,
who very actively participated and offered immense
guidance,which made this endeavour a success.
Reference :
-
http://www.evidence-based-medicine.co.uk/ebmfiles/WhatisClinGov.pdf
( Accessed on 21/11/05 )
-
Journal of diagnostic
Radiography and Imaging, Vol 4, Issue 3, 113 162.
-
http://www.ich.ucl.ac.uk/chi/guide_cg.html (
Accessed on 23/11/05)
-
http://bmj.bmjjournals.com/cgi/content/full/317/7150/61
( Accessed on 23/11/05)
-
http://bmj.bmjjournals.com/cgi/content/full/322/7299/1413?
(Accessed on 23/11/05)
-
http://www.nice.org.uk/pdf/BestPracticeClinicalAudit.pdf
(Accessed on 13/01/06)
-
http://www.rtpi.org.uk/careers-and-membership/cpd/
(Accessed on 13/01/06)
-
http://www.nice.org.uk/pdf/BestPracticeClinicalAudit.pdf
(Accessed on 13/01/06)
-
http://www.gmc-uk.org/education/pro_development/pro_development_guidance.asp
(Accessed on 13/01/06)
|